A nurse is planning care for a full-term newborn who is receiving phototherapy. Which of the following actions should the nurse include in the plan of care?
Keep the newborn supine throughout treatment.
Dress the newborn in lightweight clothing.
Measure the newborn's temperature every 8 hours.
Avoid using lotion or ointment on the newborn's skin.
The Correct Answer is D
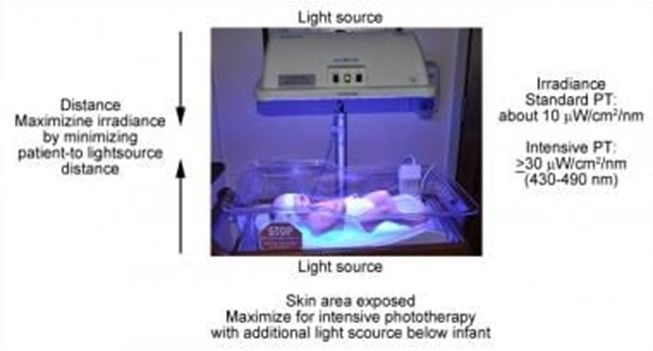
Phototherapy is a treatment that uses light to lower the level of bilirubin in the blood of newborns who have jaundice. Jaundice is a condition that causes yellowing of the skin and eyes due to high levels of bilirubin, a waste product that is normally removed by the liver. Phototherapy helps the body break down and eliminate bilirubin through urine and stool¹.
Phototherapy can be done at home or in the hospital, depending on the severity of jaundice and the type of light used. The most common types of light are fluorescent lamps, halogen lamps, or light-emitting diodes (LEDs). The light can be delivered through overhead units, fiber-optic blankets, or fiber-optic pads. The light should cover as much of the newborn's skin as possible, except for the eyes and genitals¹².
The nurse should follow certain guidelines when caring for a newborn who is receiving phototherapy, such
as:
- Monitor the newborn's temperature, hydration, weight, and urine and stool output regularly
- Protect the newborn's eyes with eye patches or goggles to prevent eye damage
- Turn the newborn every 2 to 4 hours to expose different parts of the body to the light
- Feed the newborn frequently to prevent dehydration and promote bilirubin excretion
- Check the newborn's skin color and bilirubin level periodically to evaluate the effectiveness of
phototherapy
- Provide emotional support and education to the parents about jaundice and phototherapy
One of the important guidelines is to avoid using lotion or ointment on the newborn's skin during phototherapy. This is because lotion or ointment can block the light from reaching the skin and reduce the effectiveness of phototherapy. Lotion or ointment can also cause skin irritation, rash, or burns if they react with the light. The newborn's skin should be clean and dry before phototherapy¹²³.
The other options are not actions that the nurse should include in the plan of care:
- a) Keep the newborn supine throughout treatment. This is not correct because keeping the newborn in one position can limit the exposure of different parts of the body to the light and reduce the effectiveness of phototherapy. The nurse should turn the newborn every 2 to 4 hours to expose different parts of the body to the light¹².
- b) Dress the newborn in lightweight clothing. This is not correct because dressing the newborn in clothing can block the light from reaching the skin and reduce the effectiveness of phototherapy. The newborn should be undressed except for a diaper during phototherapy¹².
- c) Measure the newborn's temperature every 8 hours. This is not correct because measuring the newborn's temperature every 8 hours may not be frequent enough to detect any changes in temperature that may occur during phototherapy. Phototherapy can cause overheating or hypothermia in newborns, depending on the type and intensity of light used. The nurse should monitor the newborn's temperature more often, such as every 2 to 4 hours, and adjust the room temperature or use blankets as needed¹².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
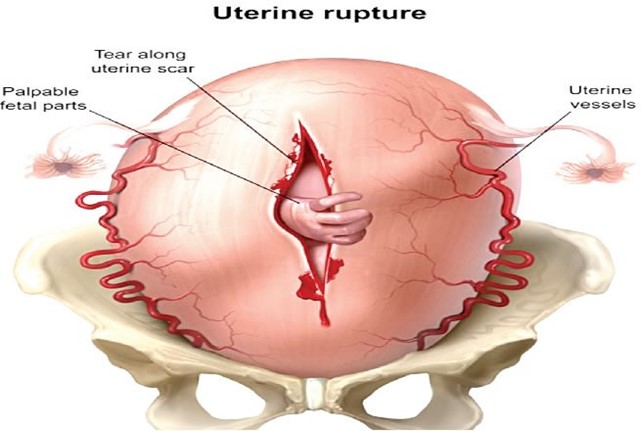
Uterine rupture is a rare but life-threatening complication of labor and delivery that occurs when the uterus tears open along the scar line of a previous cesarean delivery or other uterine surgery¹². Uterine rupture can cause severe bleeding in the mother and deprive the baby of oxygen¹². Some of the signs and symptoms of uterine rupture are:
- Sudden, severe lower abdominal pain
- Drop in blood pressure
- Cool skin and pallor
- Prolonged fetal bradycardia (slow heart rate)
- Loss of fetal station (the baby moves back up the birth canal)
- Abnormal or absent uterine contractions¹²³
Uterine rupture is a medical emergency that requires immediate surgery to deliver the baby and repair the uterus or remove it (hysterectomy)¹².
The other options are incorrect because they have different signs and symptoms:
b) Amniotic fluid embolism is a rare but serious condition that occurs when amniotic fluid or fetal cells enter the mother's bloodstream and trigger an allergic reaction. It can cause sudden respiratory distress, cardiac arrest, seizures, or coma in the mother and fetal distress or death in the baby¹². It usually occurs during labor, delivery, or shortly after birth¹².
c) Placenta previa is a condition where the placenta covers part or all of the opening of the cervix. It can cause painless vaginal bleeding during pregnancy or labor¹². It does not affect the blood pressure or fetal heart rate unless there is severe bleeding or placental abruption (separation of the placenta from the uterine wall)¹².
d) Umbilical cord prolapse is a condition where the umbilical cord slips through the cervix and into the vagina before or during labor. It can cause fetal distress, as the cord can become compressed or twisted, cutting off the blood supply and oxygen to the baby¹². It usually causes a sudden drop in fetal heart rate, but does not affect the maternal blood pressure or cause abdominal pain¹².
Correct Answer is D
Explanation
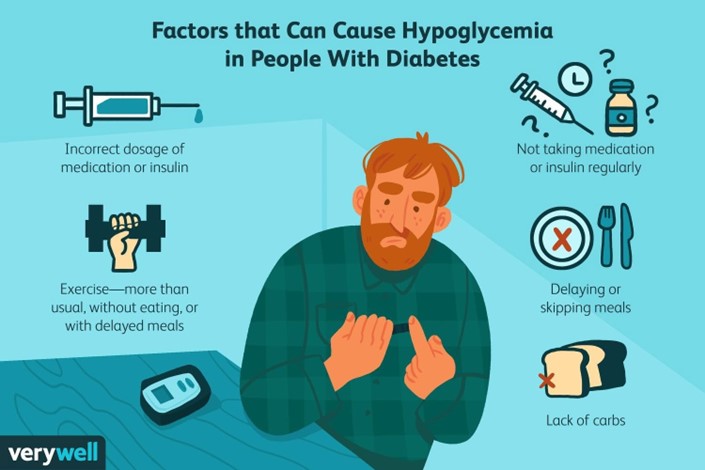
A postpartum client who has type 1 diabetes mellitus and is breastfeeding her newborn should maintain
scheduled mealtimes for herself to prevent hypoglycemia and ensure adequate milk production¹. Breastfeeding may lower glucose levels in the parent and the risk of type 1 and type 2 diabetes in the child¹. Breastfeeding may also help the parent lose weight, prevent diabetes-related complications, and reduce the chances of some cancers¹.
The other options are incorrect because:
a) Taking more insulin with each meal than you did prior to pregnancy may cause hypoglycemia, especially if you are breastfeeding. You should adjust your insulin doses according to your blood glucose levels and carbohydrate intake, and consult your doctor or diabetes educator for guidance²³.
b) Checking your blood glucose levels every 8 hours is not frequent enough to monitor your diabetes during breastfeeding. You should check your blood glucose levels before and after each breastfeeding session, as well as before meals and snacks, at bedtime, and during the night if needed²³.
c) Limiting your carbohydrate intake to 30 grams per day is too restrictive and may impair your milk production and quality, as well as cause hypoglycemia or ketoacidosis. You should consume adequate carbohydrates from healthy sources, such as whole grains, fruits, vegetables, legumes, and dairy products, to meet your energy and nutritional needs²³.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
