A nurse is assisting with the care of a client who is using pattern-paced breathing during the first stage of labor. The client says she feels lightheaded, and her fingers are tingling. Which of the following actions should the nurse take?
Instruct the client to maintain a breathing rate no less than twice the normal rate.
Administer oxygen via nasal cannula.
Assist the client to breathe into a paper bag.
Have the client tuck her chin to her chest.
The Correct Answer is C
The correct answer is choice C. Assist the client to breathe into a paper bag.
Choice A rationale:
Instructing the client to maintain a breathing rate no less than twice the normal rate is not appropriate. This could exacerbate hyperventilation, leading to further lightheadedness and tingling.
Choice B rationale:
Administering oxygen via nasal cannula is not necessary in this situation. The symptoms are due to hyperventilation, not a lack of oxygen.
Choice C rationale:
Assisting the client to breathe into a paper bag helps to rebreathe carbon dioxide, which can correct the respiratory alkalosis caused by hyperventilation. This will alleviate the symptoms of lightheadedness and tingling.
Choice D rationale:
Having the client tuck her chin to her chest is not a recognized intervention for hyperventilation. It would not address the underlying issue of respiratory alkalosis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
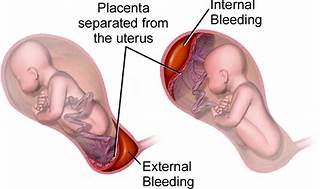
The correct answer is choice A, Maternal hypertension.
Choice A rationale:
Maternal hypertension is widely recognized as the most common risk factor for placental abruption. High blood pressure can cause the placenta to detach from the uterine wall, leading to abruption. In summary, while all the listed factors can contribute to the risk of placental abruption, maternal hypertension stands out as the most common cause, supported by multiple health sources. It’s important for nurses to recognize and manage hypertension in pregnant clients to minimize the risk of this serious complication.
Choice B rationale:
While maternal cocaine use is a significant risk factor for placental abruption due to its vasoconstrictive effects, which can compromise the placental blood flow, it is not as common as maternal hypertension.
Choice C rationale:
Maternal cigarette smoking is also a risk factor for placental abruption. Smoking can lead to a variety of complications in pregnancy, including placental problems, but again, it is less common than hypertension as a cause for abruption.
Choice D rationale:
Maternal battering can lead to trauma which may result in placental abruption. However, it is not considered the most common risk factor when compared to maternal hypertension.
Correct Answer is A
Explanation
Choice A rationale:
Supporting the infant during birth. The priority for the nurse in this situation is to ensure the safe delivery of the baby. By supporting the infant during birth, the nurse can help ensure that the baby is delivered safely and efficiently. This involves assisting the mother in pushing and guiding the baby's head and body as it emerges from the birth canal. The nurse should also be ready to catch the baby and provide immediate care, such as drying and stimulating the baby to breathe if necessary.
Choice B rationale
Preventing the perineum from tearing. While preventing perineal tearing is important, it is not the top priority in this rapidly progressing labor scenario. The immediate concern is the safe delivery of the baby, and if perineal tearing does occur, it can be addressed after the birth.
Choice C rationale
Cutting the umbilical cord. This action is necessary but not the top priority. After the baby is delivered, the nurse should clamp and cut the umbilical cord to separate the baby from the placenta. However, this can wait until the baby is fully delivered and breathing on their own.
Choice D rationale
Promoting delivery of the placenta. Again, while delivering the placenta is important to prevent postpartum haemorrhage, it is not the priority in this scenario. The nurse's immediate focus should be on supporting the infant's delivery and ensuring the baby's well-being.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
