A nurse is caring for a client 2 hours following a spontaneous vaginal delivery and notes that the client has saturated
two perineal pads with blood in a 30-minute period.
Which of the following actions should the nurse take first?
Increase the client’s fluid intake
Check the consistency of the client’s uterine fundus
Help the client use the bedpan to urinate
Prepare to administer tocolytic medication
The Correct Answer is B
Choice A rationale:
Increasing fluid intake is not the priority action in this situation. While maintaining adequate hydration is important for
postpartum recovery, it does not directly address the immediate concern of excessive bleeding. Excessive fluid intake could
potentially worsen the bleeding by increasing blood volume and potentially increasing blood pressure.
Choice C rationale:
Helping the client use the bedpan to urinate is not the priority action in this case. While a full bladder can sometimes interfere
with uterine contraction and contribute to postpartum bleeding, it is not the most likely cause of the excessive bleeding in this
scenario. The client has already saturated two perineal pads in a short period, indicating a more significant bleeding issue that
needs to be addressed first.
Choice D rationale:
Preparing to administer tocolytic medication is not the appropriate action at this time. Tocolytic medications are used to stop
contractions, but they are not typically used to manage postpartum hemorrhage. In fact, tocolytics could potentially worsen
the bleeding by interfering with the natural mechanisms that help the uterus contract and stop bleeding after delivery.
Choice B rationale:
Checking the consistency of the client's uterine fundus is the priority action in this situation. The most common cause of
postpartum hemorrhage is uterine atony, which means the uterus is not contracting effectively to clamp down on the blood
vessels where the placenta was attached. A soft, boggy fundus is a sign of uterine atony. By assessing the fundus, the nurse can
quickly determine if uterine atony is the likely cause of the bleeding and take appropriate interventions to manage it.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Evaluating the side effects of analgesia is not the priority action in this situation. While it's important to assess for potential
side effects, the client's immediate need to use the bathroom takes precedence.
Analgesia might contribute to urinary retention in some cases, but it's not the most likely reason for the client's request.
Promptly addressing the client's need to void helps prevent bladder distention, discomfort, and potential urinary tract
infections.
Choice B rationale:
Using a wheelchair is not necessary in most cases after a vaginal birth.
Early ambulation is generally encouraged to promote circulation, prevent blood clots, and aid in recovery.
Requiring a wheelchair could delay the client's ability to void and might make her feel less independent.
Choice C rationale:
Advising the client to remain in bed is not recommended practice after a vaginal birth.
Prolonged bed rest can increase the risk of complications, such as blood clots, muscle weakness, and delayed bowel function.
Early ambulation, as tolerated, is crucial for promoting physical recovery and preventing postpartum complications.
Correct Answer is D
Explanation
Choice A rationale:
Rh positive individuals already have the Rh factor on their red blood cells, so they do not need Rho(D) immune globulin to
prevent sensitization.
The newborn being Rh positive does not pose a risk to an Rh positive mother, as their blood types are compatible.
Choice B rationale:
Rh positive individuals cannot develop antibodies against the Rh factor, as it is already present on their own red blood cells.
The newborn's Rh negative status does not create a risk of sensitization for the mother, as there is no Rh factor to trigger an
immune response.
Choice C rationale:
If both the mother and the newborn are Rh negative, there is no risk of Rh incompatibility.
This is because neither individual has the Rh factor on their red blood cells, so there is no potential for sensitization.
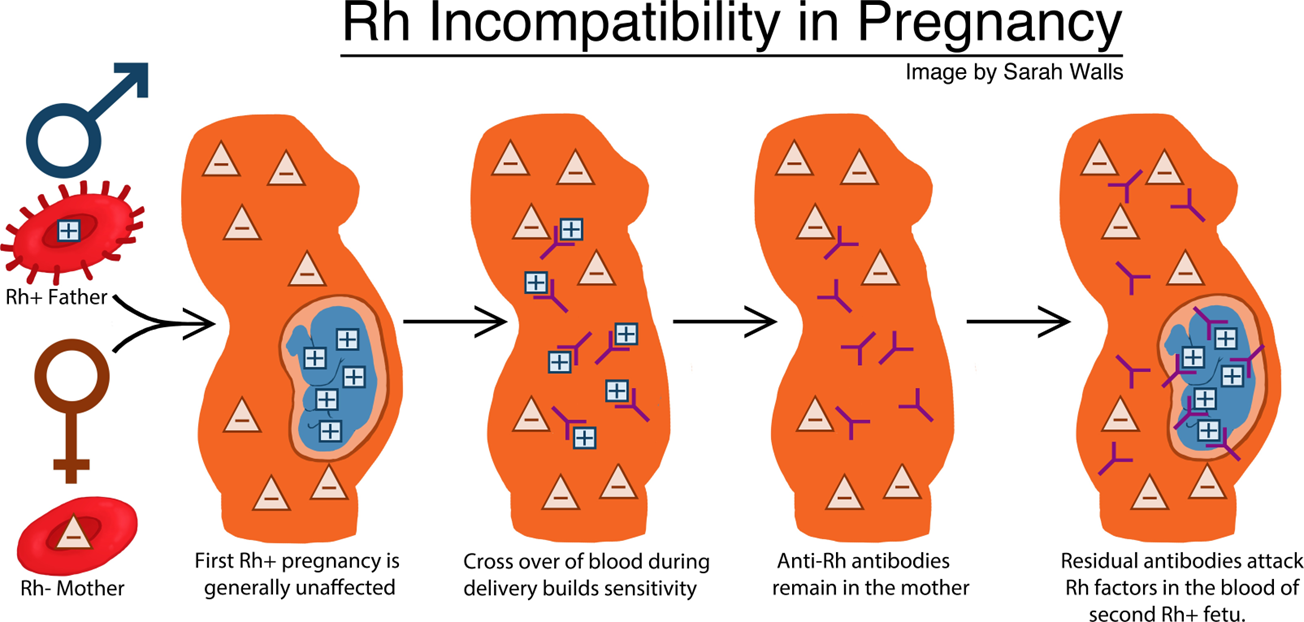
Choice D rationale:
When an Rh negative mother carries an Rh positive fetus, there is a risk of Rh sensitization during pregnancy and delivery.
This occurs when fetal blood cells cross the placenta and enter the mother's bloodstream, exposing her immune system to the
Rh factor.
If the mother's immune system recognizes the Rh factor as foreign, it can produce antibodies against it.
These antibodies can cross the placenta in subsequent pregnancies and attack the red blood cells of Rh positive fetuses,
leading to hemolytic disease of the newborn (HDN).
Rho(D) immune globulin is a medication that can prevent Rh sensitization by binding to Rh positive fetal blood cells that have
entered the mother's bloodstream.
This prevents the mother's immune system from recognizing the Rh factor and producing antibodies.
Rho(D) immune globulin is typically given to Rh negative mothers within 72 hours of delivery of an Rh positive newborn, as well as after other events that could lead to Rh sensitization, such as miscarriage, abortion, or ectopic pregnancy.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
