A nurse is caring for a client who has bulimia nervosa.
The client is at risk for developing
The Correct Answer is {"dropdown-group-1":"D","dropdown-group-2":"D"}
Cardiovascular abnormalities are a serious risk in clients with bulimia nervosa due to electrolyte imbalances, especially hypokalemia, which can lead to arrhythmias, weakened heart muscles, and potential heart failure. Hyponatremia (low sodium levels) can occur due to excessive vomiting, which leads to the loss of fluids and electrolytes, including sodium. Incorrect responses: Group 1: Hypoglycemia: Bulimia nervosa primarily causes electrolyte imbalances and acid-base disturbances due to vomiting, not significant alterations in blood sugar levels. Metabolic Acidosis: Vomiting leads to the loss of gastric acid, causing metabolic alkalosis. Hypotension: Hypotension could occur if the client experiences significant dehydration from vomiting. Hypotension would be a consequence of severe dehydration rather than a primary risk at this stage. Hyperglycemia: Hyperglycemia is not typically associated with bulimia nervosa or vomiting. It would be more relevant in conditions like diabetes. Group 2: Hyperkalemia: Hyperkalemia (high potassium) is unlikely in bulimia nervosa, where frequent vomiting usually leads to hypokalemia due to the loss of potassium in gastric secretions. Metabolic Acidosis: As mentioned before, vomiting leads to metabolic alkalosis, not acidosis, because of the loss of hydrochloric acid. Hypochloremia: Hypochloremia (low chloride levels) can occur with vomiting due to the loss of stomach acid, which contains chloride. While it is a possible outcome, metabolic alkalosis better captures the overall acid-base disturbance in the client.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Clean the mouthpiece with warm water every 2 weeks. This is incorrect because the mouthpiece should be cleaned with warm water at least once a week, or more often if used frequently, to prevent bacterial growth and contamination.
B. Wait 10 seconds between inhalations. This is incorrect because the recommended time interval between inhalations is 1 minute, not 10 seconds, to allow adequate absorption of the medication and prevent overdose or side effects.
C. Take a quick inhalation when pressing the dispenser. This is incorrect because a quick inhalation can cause poor coordination of hand-mouth movement and result in less medication reaching the lungs. The nurse should instruct the child to take a slow, deep inhalation when pressing the dispenser, hold their breath for 10 seconds, and exhale slowly.
D. Take the medication 15 min before playing sports. This is correct because albuterol is a short-acting bronchodilator that can prevent exercise-induced bronchospasm. The nurse should teach the child to take the medication before engaging in physical activity that can trigger asthma symptoms, such as sports, cold weather, or allergens.
Correct Answer is A
Explanation
Choice A reason:
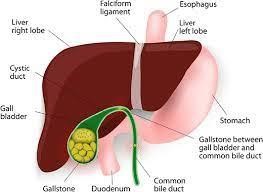
Acetaminophen is a safer choice for pain relief in clients with cholelithiasis because it does not have significant effects on the gallbladder or biliary system. It can provide effective pain relief without exacerbating the underlying condition.
Choice B reason:
Omeprazole Omeprazole should not administer because it is a proton pump inhibitor (PPI) used to reduce stomach acid production and treat conditions such as gastroesophageal reflux disease (GERD) and peptic ulcers. It is not indicated for the treatment of pain and discomfort associated with cholelithiasis.
Choice C reason
Should not be administered
Metoclopramide Metoclopramide should not be administered because it is a medication used to treat gastrointestinal issues such as nausea, vomiting, and gastroparesis. It is not indicated for the treatment of pain associated with cholelithiasis.
Choice D reason:
Ketorolac Ketorolac should not be administered because it is an NSAID used for moderate to severe pain. However, it should be avoided in clients with cholelithiasis due to its potential adverse effects on the gallbladder and biliary system.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
