A nurse is caring for a client who has preeclampsia and is receiving magnesium sulfate. Which of the following clinical findings should the nurse instruct the client to report?
Increased respiratory rate
Increased fetal movement
Increased urinary output
Increased muscle weakness
The Correct Answer is D
When caring for a client with preeclampsia receiving magnesium sulfate, the nurse should instruct the client to report any increased muscle weakness. Magnesium sulfate is a medication commonly used to prevent and treat seizures in clients with preeclampsia. However, one of the side effects of magnesium sulfate is muscle weakness. If the client experiences an increase in muscle weakness, it could indicate magnesium toxicity, which requires immediate medical attention.
Option a) Increased respiratory rate is not typically associated with magnesium sulfate administration. However, respiratory depression is a potential side effect, so a decreased respiratory rate should be reported.
Option b) Increased fetal movement is generally considered a positive sign of fetal well-being and is not a concern that needs to be reported.
Option c) Increased urinary output is not typically a concerning finding. In fact, maintaining adequate urine output is desired in clients with preeclampsia to ensure proper kidney function. However, a sudden decrease in urinary output or signs of dehydration should be reported.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
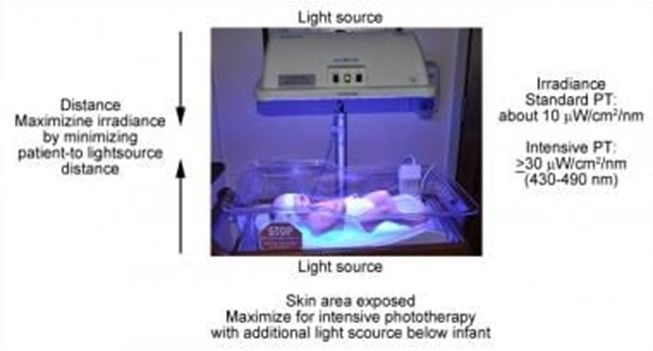
Phototherapy is a treatment that uses light to lower the level of bilirubin in the blood of newborns who have jaundice. Jaundice is a condition that causes yellowing of the skin and eyes due to high levels of bilirubin, a waste product that is normally removed by the liver. Phototherapy helps the body break down and eliminate bilirubin through urine and stool¹.
Phototherapy can be done at home or in the hospital, depending on the severity of jaundice and the type of light used. The most common types of light are fluorescent lamps, halogen lamps, or light-emitting diodes (LEDs). The light can be delivered through overhead units, fiber-optic blankets, or fiber-optic pads. The light should cover as much of the newborn's skin as possible, except for the eyes and genitals¹².
The nurse should follow certain guidelines when caring for a newborn who is receiving phototherapy, such
as:
- Monitor the newborn's temperature, hydration, weight, and urine and stool output regularly
- Protect the newborn's eyes with eye patches or goggles to prevent eye damage
- Turn the newborn every 2 to 4 hours to expose different parts of the body to the light
- Feed the newborn frequently to prevent dehydration and promote bilirubin excretion
- Check the newborn's skin color and bilirubin level periodically to evaluate the effectiveness of
phototherapy
- Provide emotional support and education to the parents about jaundice and phototherapy
One of the important guidelines is to avoid using lotion or ointment on the newborn's skin during phototherapy. This is because lotion or ointment can block the light from reaching the skin and reduce the effectiveness of phototherapy. Lotion or ointment can also cause skin irritation, rash, or burns if they react with the light. The newborn's skin should be clean and dry before phototherapy¹²³.
The other options are not actions that the nurse should include in the plan of care:
- a) Keep the newborn supine throughout treatment. This is not correct because keeping the newborn in one position can limit the exposure of different parts of the body to the light and reduce the effectiveness of phototherapy. The nurse should turn the newborn every 2 to 4 hours to expose different parts of the body to the light¹².
- b) Dress the newborn in lightweight clothing. This is not correct because dressing the newborn in clothing can block the light from reaching the skin and reduce the effectiveness of phototherapy. The newborn should be undressed except for a diaper during phototherapy¹².
- c) Measure the newborn's temperature every 8 hours. This is not correct because measuring the newborn's temperature every 8 hours may not be frequent enough to detect any changes in temperature that may occur during phototherapy. Phototherapy can cause overheating or hypothermia in newborns, depending on the type and intensity of light used. The nurse should monitor the newborn's temperature more often, such as every 2 to 4 hours, and adjust the room temperature or use blankets as needed¹².
Correct Answer is B
Explanation
When providing postpartum care teaching to a client, the nurse should include accurate and appropriate information. Option b) "You can expect your breasts to be firm and tender 3 to 5 days after delivery" is a correct statement.
Breast engorgement is a common occurrence around the third to fifth day after delivery as the breasts transition from producing colostrum to mature milk. This can cause the breasts to become firm, swollen, and tender. It is important for the client to be aware of this normal physiological change and to understand how to manage it effectively, such as by applying warm or cold compresses, expressing milk, and ensuring proper breastfeeding techniques.
Option a) "Your bleeding will remain bright red for the next 6 to 8 weeks" is an incorrect statement. After childbirth, the bleeding, called lochia, typically progresses from bright red to a pinkish color and then to a yellowish-white discharge. The duration and characteristics of lochia can vary for each individual, but it generally resolves within a few weeks.
Option c) "You don't need to use birth control if you are exclusively breastfeeding" is an incorrect statement. While breastfeeding can provide some natural contraception, it is not foolproof, and the client can still ovulate and become pregnant. It is important for the client to discuss and choose a suitable method of contraception with her healthcare provider.
Option d) "You should begin performing Kegel exercises 6 to 7 weeks after delivery" is an incorrect statement. Kegel exercises, which strengthen the pelvic floor muscles, can be started as early as the immediate postpartum period and are beneficial for promoting bladder and bowel control, as well as aiding in postpartum recovery. The client can begin performing Kegel exercises soon after delivery, as guided by her healthcare provider.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
