A nurse is caring for a client who reports a new onset of severe chest pain. Which of the following actions should the nurse take to determine if the client is experiencing a myocardial infarction?
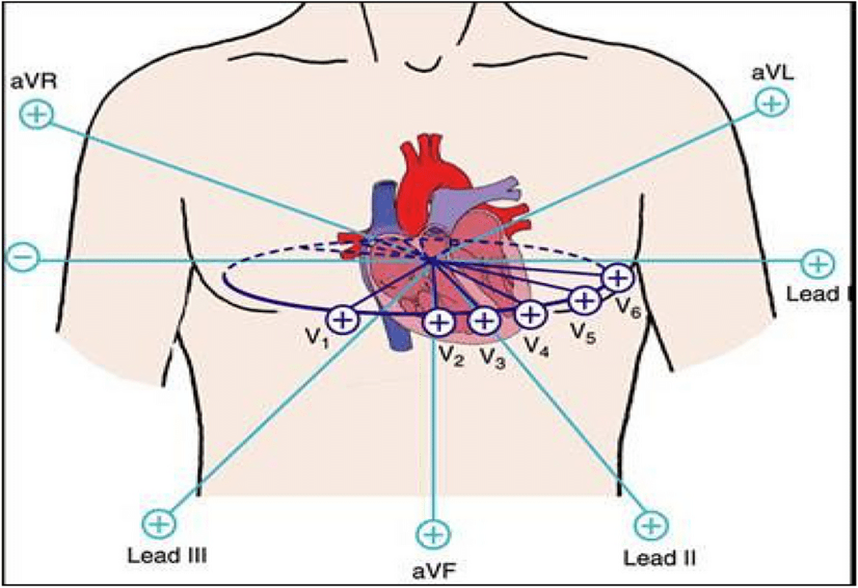
Perform a 12-lead ECG
Determine if pain radiates to the left arm
Check the client's blood pressure
Auscultate heart tones
The Correct Answer is A
Choice A reason: A 12-lead ECG can reveal changes in the ST segment, T wave, and QRS complex, which are indicative of myocardial ischemia, injury, or infarction. It is the first line diagnostic test that needs to be recorded within 10 minutes after the first medical contact in cases of suspected acute coronary syndromes.
Choice B reason: While pain radiating to the left arm can be a symptom of MI, it is not a definitive diagnostic action. It is a common symptom but can also be associated with other conditions.
Choice C reason: Checking the client's blood pressure is important in the overall assessment of the client's cardiovascular status but does not specifically diagnose MI. Blood pressure can be normal, elevated, or decreased in the case of MI.
Choice D reason: Auscultating heart tones can provide information about the presence of murmurs, gallops, or rubs, but it is not a specific diagnostic action for MI. Heart sounds may be normal during an MI.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","C"]
Explanation
Tachycardia, or a rapid heartbeat, is a common response to the pain and stress associated with stomach perforation. The body’s sympathetic nervous system is activated in response to the pain and the potential shock state due to internal bleeding or infection, leading to an increased heart rate. Tachycardia is also a compensatory mechanism to maintain adequate blood flow and oxygen delivery to vital organs in the setting of decreased blood volume. A stomach perforation due to a peptic ulcer is a serious medical condition where an ulcer has led to a hole in the stomach lining. This can lead to the contents of the stomach spilling into the abdominal cavity, causing peritonitis, which is an inflammation of the peritoneum (the lining of the abdominal cavity).
Choice B: Rebound tenderness
Rebound tenderness is a clinical sign that indicates irritation of the peritoneum. When pressure is applied to the abdomen and then quickly released, the sudden movement of the peritoneal layers against each other produces sharp, rebound pain. This is a classic sign of peritonitis, which can occur with stomach perforation as gastric contents irritate the peritoneum. When assessing a client with a suspected stomach perforation due to a peptic ulcer, a nurse should expect to find signs of tachycardia, rebound tenderness, and a rigid abdomen. These findings are indicative of the body’s response to the acute abdominal condition and peritoneal irritation. It is crucial to recognize these signs promptly as stomach perforation is a medical emergency requiring immediate intervention.
Choice C: Rigid abdomen
A rigid abdomen is indicative of involuntary guarding, a reflex contraction of the abdominal muscles to protect inflamed organs within the abdomen. This rigidity is a sign of peritoneal irritation and is often present in cases of stomach perforation. The rigidity helps to immobilize the area, which may reduce pain but also serves as a clinical indicator of serious intra-abdominal pathology.
Choice D: Elevated blood pressure
Elevated blood pressure is not typically a direct result of stomach perforation. In fact, blood pressure may initially be normal or even low, depending on the body’s response to internal bleeding and the potential development of shock. However, pain and anxiety can cause a transient increase in blood pressure, but it is not a primary diagnostic criterion for stomach perforation.
Correct Answer is D
Explanation
Choice A reason:Atrial fibrillation is not typically treated with defibrillation; it is usually managed with medication or other forms of rhythm control.
Choice B reason:Supraventricular tachycardia does not usually require defibrillation; it may be treated with vagal maneuvers or medication.
Choice C reason:Asystole, or the absence of a heartbeat, is not treated with defibrillation as there is no electrical activity to reset.
Choice D reason:Ventricular fibrillation is a life-threatening heart rhythm that requires immediate defibrillation to restore a normal heart rhythm.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
