A nurse is caring for a toddler who is 24 hours postoperative following a cleft palate repair. Which of the following actions should the nurse take?
Apply bilateral wrist restraints.
Administer opioids for pain.
Implement a soft diet.
Offer fluids through a straw.
The Correct Answer is C
Choice A reason: Apply Bilateral Wrist Restraints
Applying bilateral wrist restraints can be necessary in some cases to prevent the child from touching or interfering with the surgical site. However, restraints should be used as a last resort and only when absolutely necessary. They can cause distress and discomfort to the child and should be monitored closely to prevent any complications.
Choice B reason: Administer Opioids for Pain
Administering opioids for pain management is a common practice post-surgery to ensure the child is comfortable. However, opioids should be used cautiously due to the risk of side effects and potential for dependency. Non-opioid pain management strategies, such as acetaminophen or ibuprofen, are often preferred unless the pain is severe.
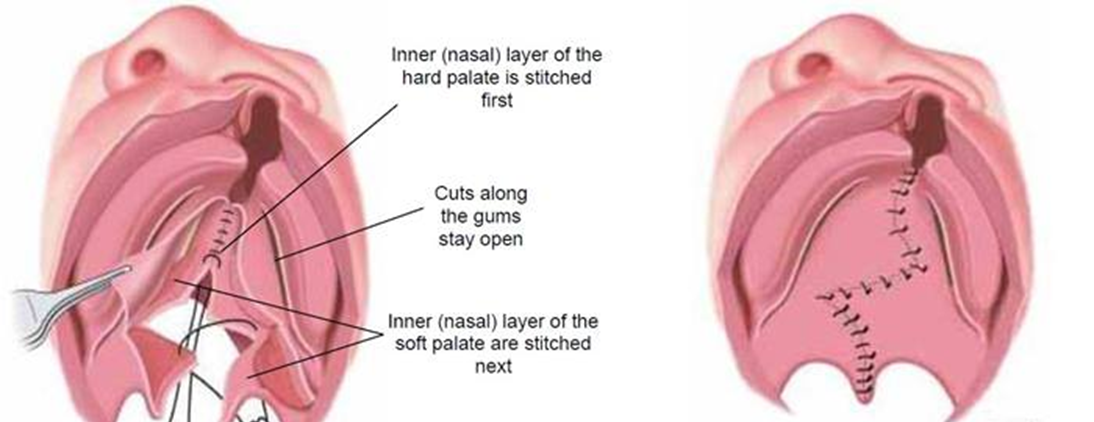
Choice C reason: Implement a Soft Diet
Implementing a soft diet is crucial for a child who is 24 hours postoperative following a cleft palate repair. The surgical site in the mouth is still healing, and a soft diet helps prevent any damage or irritation to the area. Soft foods are easier to swallow and less likely to cause pain or disrupt the healing process. Examples of soft foods include mashed potatoes, yogurt, and pureed fruits.
Choice D reason: Offer Fluids Through a Straw
Offering fluids through a straw is not recommended for a child who has undergone cleft palate repair. The suction created by using a straw can put pressure on the surgical site and potentially cause complications. Instead, fluids should be offered using a cup or a spoon to minimize any risk to the healing palate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason: Airborne
Airborne precautions are used for diseases that are transmitted through tiny airborne particles that can remain suspended in the air and be inhaled by others. Examples of diseases requiring airborne precautions include tuberculosis, measles, and chickenpox. These diseases can spread over long distances and through ventilation systems. Pertussis, however, is not transmitted via airborne particles but rather through larger respiratory droplets.
Choice B reason: Contact
Contact precautions are used for infections that are spread by direct or indirect contact with the patient or the patient’s environment. This includes infections like methicillin-resistant Staphylococcus aureus (MRSA) and Clostridioides difficile (C. diff). While contact precautions are important for preventing the spread of certain infections, pertussis is primarily spread through respiratory droplets, making droplet precautions more appropriate.
Choice C reason: Protective
Protective precautions, also known as reverse isolation, are used to protect immunocompromised patients from potential infections. This type of precaution is not intended to prevent the spread of infections from the patient to others but rather to protect the patient from external sources of infection. Examples include patients undergoing chemotherapy or those with severe immunodeficiency. Pertussis does not require protective precautions as it is not about protecting the patient from others.
Choice D reason: Droplet
Droplet precautions are the appropriate transmission-based precautions for pertussis. Pertussis, also known as whooping cough, is spread through respiratory droplets that are produced when an infected person coughs, sneezes, or talks. These droplets can travel short distances and can infect others who are in close proximity. Droplet precautions include wearing a mask when within 3 feet of the patient, placing the patient in a private room if possible, and ensuring that the patient wears a mask if they need to be transported.
Correct Answer is A
Explanation
Choice A reason: Administer the Medications 5 Minutes Apart
Administering the medications 5 minutes apart is crucial when using multiple eye drops. This practice ensures that each medication has enough time to be absorbed without being washed out by the subsequent drop. This is particularly important for medications like timolol and pilocarpine, which are used to manage intraocular pressure in glaucoma.
Choice B reason: Hold Pressure on the Conjunctival Sac for 2 Minutes Following Application of Drops
Holding pressure on the conjunctival sac (punctal occlusion) for 2 minutes after applying eye drops can help reduce systemic absorption and increase the local effect of the medication. However, this instruction is not as critical as the timing between administering different eye drops.
Choice C reason: It Is Not Necessary to Remove Contact Lenses Before Administering Medications
This statement is incorrect. Contact lenses should be removed before administering eye drops to prevent contamination and ensure proper absorption of the medication. The lenses can be reinserted after a sufficient amount of time has passed, usually around 15 minutes.
Choice D reason: Administer the Medications by Touching the Tip of the Dropper to the Sclera of the Eye
This statement is incorrect. The tip of the dropper should never touch the eye or any other surface to avoid contamination. The correct method is to hold the dropper above the eye and squeeze out the prescribed number of drops into the conjunctival sac.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
