A nurse is contributing to the plan of care for a client who has a seizure disorder. Which of the following interventions should the nurse include in the plan? (Select all that apply.)
Provide a suction setup at the bedside.
Elevate the side rails when in bed.
Place a bite stick at the bedside.
Keep an oxygen setup at the bedside.
Furnish restraints at the bedside.
Correct Answer : A,B,D
A. Provide a suction setup at the bedside:
This is a relevant intervention as it ensures that suction equipment is readily available in case the client experiences excessive secretions or vomiting during or after a seizure. It helps maintain a clear airway and prevent aspiration.
B. Elevate the side rails when in bed:
Elevating the side rails can help ensure the client's safety during a seizure by preventing falls from the bed. It is a preventive measure to minimize the risk of injury.
C. Place a bite stick at the bedside:
Placing a bite stick at the bedside is not a recommended intervention. Bite sticks can potentially injure the patient's teeth or mouth during a seizure and are generally not recommended in current practice.
D. Keep an oxygen setup at the bedside:
This is an appropriate intervention as it ensures that oxygen is readily available in case the client experiences respiratory distress or hypoxia during or after a seizure. Oxygen therapy may be needed to support respiratory function.
E. Furnish restraints at the bedside:
Furnishing restraints at the bedside is not a recommended intervention for managing seizures. Restraints should only be used in exceptional circumstances when the client's safety or the safety of others is at risk and should be applied according to institutional policies and legal regulations.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Difficulty initiating speech
This is a characteristic symptom of expressive aphasia. Individuals with expressive aphasia have difficulty initiating speech and may produce speech that is slow, effortful, and lacking in grammatical structure.
B. Difficulty understanding the written and spoken word
This symptom is not typically associated with expressive aphasia. Instead, difficulty understanding language, both written and spoken, is more commonly seen in receptive aphasia, also known as Wernicke's aphasia.
C. Total inability to communicate
While expressive aphasia can severely impair verbal communication, it does not result in a total inability to communicate. Individuals with expressive aphasia may still be able to communicate to some extent using nonverbal means, gestures, or writing.
D. Stuttering and spitting
Stuttering and spitting are not characteristic symptoms of expressive aphasia. Stuttering is a speech disorder characterized by interruptions in the flow of speech, while spitting is not typically associated with aphasia.
Correct Answer is C
Explanation
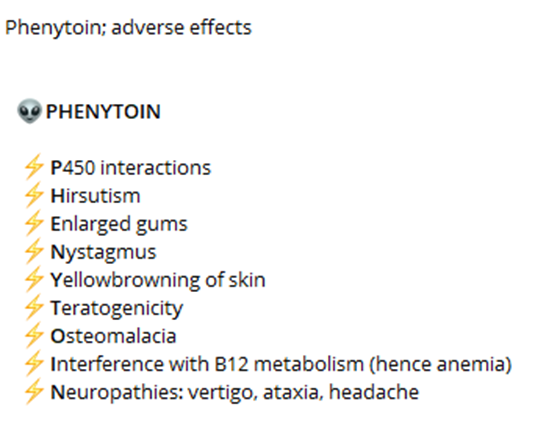
A. Diarrhea:
Diarrhea is not a common side effect of phenytoin. While gastrointestinal disturbances such as nausea, vomiting, and constipation may occur, diarrhea is less common. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
B. Wrist pain:
Wrist pain is not a common side effect of phenytoin. Side effects related to musculoskeletal issues such as joint pain, muscle weakness, or muscle twitching can occur, but wrist pain specifically is not commonly associated with phenytoin use. Therefore, it is not a primary adverse effect that the nurse should instruct the client to monitor and report.
C. Skin rash:
Skin rash is a potential adverse effect of phenytoin that should be monitored and reported. Phenytoin can cause various skin reactions, including a mild rash or more severe reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis. Therefore, the nurse should instruct the client to promptly report any signs of skin rash or other skin changes.
D. Metallic taste:
Metallic taste is a common side effect of phenytoin. While it is not usually a serious adverse effect, it can be bothersome for some individuals. Therefore, the nurse should instruct the client to monitor for this side effect and report it if it occurs persistently or becomes bothersome.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
