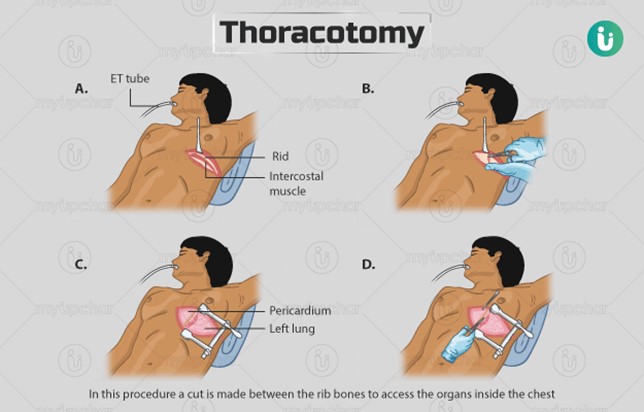
A nurse is observing the closed chest drainage system of a client who is 24 hr post thoracotomy. The nurse notes slow, steady bubbling in the suction control chamber. Which of the following actions should the nurse take?
Continue to monitor the client's respiratory status.
Check the suction control outlet on the wall.
Clamp the chest tube.
Check the tubing connections for leaks.
The Correct Answer is A
Choice A Reason: This choice is correct because slow, steady bubbling in the suction control chamber indicates that the suction is working properly and maintaining a negative pressure in the pleural space. The nurse should continue to monitor the client's respiratory status, such as breath sounds, oxygen saturation, and respiratory rate, to assess the effectiveness of the chest drainage system.
Choice B Reason: This choice is incorrect because checking the suction control outlet on the wall is not necessary unless there is no bubbling in the suction control chamber, which would indicate a problem with the suction source or setting. The nurse should ensure that the suction control outlet is set at the prescribed level, usually between 10 and 20 cm H2O.
Choice C Reason: This choice is incorrect because clamping the chest tube is not indicated unless there is a leak in the system or the chest drainage unit needs to be changed. Clamping the chest tube may cause a buildup of air or fluid in the pleural space, which can lead to tension pneumothorax or pleural effusion.
Choice D Reason: This choice is incorrect because checking the tubing connections for leaks is not necessary unless there is continuous bubbling in the water seal chamber, which would indicate an air leak in the system. The nurse should ensure that all tubing connections are tight and secure, and tape any loose connections.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: This is incorrect because the laboratory values are not within the expected reference range in a client who has DIC. DIC is a condition that causes abnormal activation of the clotting cascade, leading to widespread microthrombi formation and consumption of clotting factors and platelets. This results in bleeding complications and organ dysfunction.
Choice B Reason: This is correct because the laboratory values are prolonged in a client who has DIC. PT, aPTT, and INR are tests that measure the time it takes for blood to clot. PT measures the extrinsic pathway, aPTT measures the intrinsic pathway, and INR is a standardized ratio of PT. In DIC, these tests are prolonged because of the depletion of clotting factors and platelets.
Choice C Reason: This is incorrect because the laboratory values are not the same as the previous test values in a client who has DIC. DIC is an acute and dynamic condition that can change rapidly depending on the underlying cause and treatment. The laboratory values may fluctuate between normal, prolonged, or shortened depending on the balance between clotting and bleeding.
Choice D Reason: This is incorrect because the laboratory values are not decreased in a client who has DIC. Decreased laboratory values would indicate a shortened clotting time, which can occur in some cases of DIC when there is excessive clotting and thrombosis. However, this is not the typical finding in DIC, as most clients present with bleeding manifestations and prolonged clotting time.
Correct Answer is C
Explanation
Choice A Reason: This is incorrect because a pneumothorax is a condition in which air enters the pleural space and causes the lung to collapse. It does not cause the chest wall to move inward and outward paradoxically.
Choice B Reason: This is incorrect because atelectasis is a condition in which alveoli collapse and cause reduced gas exchange. It does not cause the chest wall to move inward and outward paradoxically.
Choice C Reason: This is correct because flail chest is a condition in which multiple ribs are fractured and cause a segment of the chest wall to detach from the rest of the thoracic cage. It causes the chest wall to move inward and outward paradoxically, as well as dyspnea and pain.
Choice D Reason: This is incorrect because a hemothorax is a condition in which blood enters the pleural space and causes the lung to collapse. It does not cause the chest wall to move inward and outward paradoxically.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
