A nurse is planning care for a newborn who is scheduled to start phototherapy using a lamp. Which of the following actions should the nurse include in the plan?
Give the newborn 1 oz of glucose water every 4 hours.
Apply a thin layer of lotion to the newborn's skin every 8 hours.
Ensure the newborn's eyes are closed beneath the shield.
Dress the newborn in a thin layer of clothing during therapy.
The Correct Answer is C
Phototherapy is a treatment method used to reduce high levels of bilirubin in the blood of a newborn with jaundice. During phototherapy, the newborn is exposed to special lights that help break down the bilirubin and allow it to be eliminated from the body. It is important to protect the newborn's eyes during phototherapy.
Option a) Giving the newborn 1 oz of glucose water every 4 hours is not necessary for phototherapy. The primary goal of phototherapy is to treat jaundice, and providing glucose water is not directly related to this treatment.
Option b)Applying a thin layer of lotion to the newborn's skin every 8 hours is not necessary during phototherapy. In fact, it is generally recommended to avoid applying lotions or oils to the skin during phototherapy as they can interfere with the effectiveness of the treatment.
Option c) Ensuring the newborn's eyes are closed beneath the shield is essential during phototherapy. The eyes are particularly sensitive to the light used in phototherapy, and exposure to the light can potentially damage the eyes. Therefore, the newborn's eyes should be protected with a shield or eye patches to prevent direct exposure to the light.
Option d) Dressing the newborn in a thin layer of clothing during therapy is appropriate. The newborn should be dressed in a way that allows as much of their skin as possible to be exposed to the phototherapy lights. This usually involves removing unnecessary clothing and covering the genital area with a diaper, while the rest of the body is exposed to the light.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Breast development is a normal part of fetal and neonatal growth. It occurs in stages, starting before birth and continuing during puberty and adulthood. Breast development is influenced by hormones, such as estrogen and progesterone, that are produced by the ovaries or the placenta¹².
Breast development in newborns can vary depending on the gestational age, sex, weight, and exposure to maternal hormones. Some newborns may have palpable breast tissue at birth, while others may develop it later in the first weeks of life. Some newborns may also secrete milk from their breasts, which is called witch's milk or neonatal galactorrhea. This is a harmless and temporary phenomenon that usually resolves within a few weeks without treatment³⁴.
The degree of breast development in newborns can be assessed by using a scoring system that ranges from 0 to 5, based on the size of the areola (the dark area around the nipple) and the presence of a bud (a small lump of glandular tissue under the areola). The scoring system is as follows³:
- Score 0: No breast tissue; flat areola with no bud
- Score 1: Breast tissue < 5 mm; flat areola with no bud
- Score 2: Breast tissue 5 to 10 mm; flat areola with no bud
- Score 3: Breast tissue > 10 mm; raised areola with no bud
- Score 4: Breast tissue > 10 mm; raised areola with bud
- Score 5: Breast tissue > 10 mm; raised areola with large bud
The average score for term newborns is 2.5 for girls and 2.0 for boys. The score tends to be higher for heavier babies and lower for lighter babies. The score also tends to be higher for babies who were exposed to higher levels of maternal hormones during pregnancy, such as those whose mothers had diabetes, preeclampsia, or multiple gestation³⁴.
A score of 0 indicates that there is no breast tissue at all, and the areola is flat with no bud. This finding can indicate preterm gestational age, as breast development usually starts before birth and progresses with increasing gestational age. Preterm newborns may have delayed or incomplete breast development due to insufficient exposure to maternal hormones or immature development of their own hormonal system³⁵.
Therefore, the nurse should identify this finding as indicating preterm gestational age and monitor the newborn for any other signs of prematurity, such as low birth weight, small head size, thin skin, low body temperature, respiratory distress, or feeding difficulties. The nurse should also provide appropriate care and support to the newborn and the parents according to the hospital protocol³⁵.
- b) Ambiguous secondary sex characteristics are physical features that do not clearly match the typical male or female pattern, such as genitalia, hair distribution, or voice pitch. They can be caused by genetic disorders, hormonal imbalances, or environmental influences. Ambiguous secondary sex characteristics do not affect breast development in newborns, as breast tissue is present in both sexes and is influenced by maternal hormones rather than sex hormones¹ .
- c) Decreased maternal hormones during pregnancy can affect breast development in newborns, but not in the way described. Decreased maternal hormones during pregnancy can cause lower breast scores in newborns, as they may have less stimulation of their breast tissue from the placenta. However, this does not mean that they have no breast tissue at all or a flat areola with no bud. They may still have some degree of breast development depending on their gestational age, sex, weight, and exposure to their own hormones³⁴.
- d) Congenital anomaly is a term that refers to any structural or functional abnormality that is present at birth. Congenital anomalies can affect any part of the body and can have various causes, such as genetic mutations, chromosomal abnormalities, infections, drugs, or environmental factors. Congenital anomalies can affect breast development in newborns, but not in the way described. Congenital anomalies that affect breast development in newborns usually cause abnormal or absent nipples or breasts, such as nipple hypoplasia (underdeveloped nipples), athelia (absence of nipples), amastia (absence of breasts), or polymastia (extra breasts). These anomalies do not cause a flat areola with no bud .
Correct Answer is C
Explanation
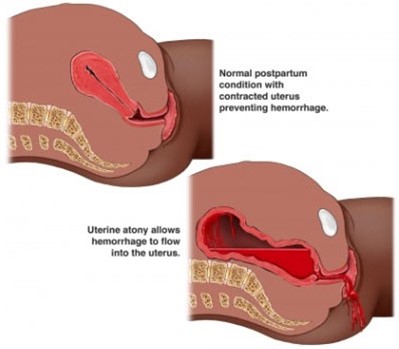
Postpartum hemorrhage (PPH) is severe vaginal bleeding after childbirth. It can occur within 24 hours of delivery (primary PPH) or up to 12 weeks postpartum (secondary PPH) ¹. PPH can cause serious complications and even death if not treated promptly and effectively¹.
The client in the question is at risk for PPH because she has a rapid labor and a high degree of cervical dilation. These factors can cause uterine atony, which is the failure of the uterus to contract and compress the blood vessels after delivery. Uterine atony is the most common cause of PPH, accounting for up to 80% of cases². Other risk factors for PPH include placental abruption, placenta previa, overdistended uterus, multiple pregnancy, prolonged labor, operative delivery, retained placenta, coagulation disorders, and infection²³.
a) Hyperemesis gravidarum is a condition of severe nausea and vomiting during pregnancy that can cause dehydration, electrolyte imbalance, weight loss, and nutritional deficiencies. It usually occurs in the first trimester and resolves by the second trimester. It is not related to PPH⁴.
b) Ectopic pregnancy is a condition where the fertilized egg implants outside the uterus, usually in the fallopian tube. It can cause abdominal pain, vaginal bleeding, and rupture of the tube. It is a medical emergency that requires prompt diagnosis and treatment. It occurs in early pregnancy and cannot be diagnosed at 12 weeks of gestation by amniocentesis.
d) Incompetent cervix is a condition where the cervix dilates prematurely and painlessly during pregnancy, leading to preterm labor and delivery or pregnancy loss. It usually occurs in the second trimester and can be treated with cervical cerclage or progesterone. It is not associated with PPH.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
