A nurse is providing education to a client in the first trimester of pregnancy. What information should the nurse include regarding the cause of indigestion and heartburn?
Increased pancreatic activity during pregnancy causes fat intolerance.
Increased estrogen production causes more hydrochloric acid in the stomach.
Pressure from the growing uterus pushes up on the stomach and intestines.
Progesterone causes relaxation of the cardiac sphincter allowing acid to reflux.
The Correct Answer is D
Choice A rationale:
Increased pancreatic activity during pregnancy causing fat intolerance is not related to the cause of indigestion and heartburn. Pancreatic activity can change during pregnancy, but it does not directly impact indigestion and heartburn.
Choice B rationale:
Increased estrogen production causing more hydrochloric acid in the stomach is not the cause of indigestion and heartburn during pregnancy. While hormones can influence digestion, the mechanism for indigestion and heartburn lies elsewhere.
Choice C rationale:
Pressure from the growing uterus pushing up on the stomach and intestines is a contributing factor to indigestion and heartburn during pregnancy. However, it is not the primary cause. The main cause is related to the relaxation of the cardiac sphincter.
Choice D rationale:
Progesterone causes relaxation of the cardiac sphincter, which is a muscular valve that prevents stomach acid from flowing back into the esophagus. When this sphincter relaxes, it can lead to acid reflux and subsequent indigestion and heartburn during pregnancy. The nurse should educate the client about this hormonal effect to help manage these symptoms effectively.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice C rationale:
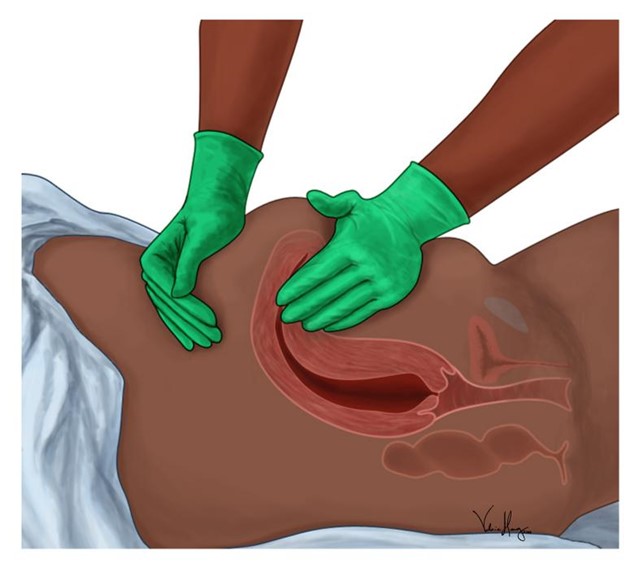
The nurse should first massage the client's fundus to address the excessive vaginal bleeding. Massaging the fundus helps the uterus contract and prevents further bleeding. Excessive postpartum bleeding may indicate uterine atony, which is a leading cause of postpartum hemorrhage. The nurse should apply gentle pressure to the fundus to promote uterine contractions and reduce bleeding.
Choice A rationale:
Elevating the client's legs to a 30° angle (Trendelenburg position) is not the priority action in this situation. Fundal massage takes precedence because it directly addresses the cause of the excessive bleeding. While Trendelenburg position might be used in some situations to increase blood flow to vital organs, it is not the first-line intervention for postpartum bleeding.
Choice B rationale:
Inserting an indwelling urinary catheter is not the priority action for excessive vaginal bleeding. While monitoring urine output is essential, the immediate concern is controlling the bleeding by massaging the fundus.
Choice D rationale:
Initiating an infusion of oxytocin may be indicated if fundal massage alone is insufficient to control bleeding. However, massaging the fundus should be the first action taken to promote uterine contractions. Oxytocin can be administered afterward, if needed, under the direction of a healthcare provider.
Correct Answer is B
Explanation
Choice A rationale:
Hyporeactivity is not typically associated with neonatal abstinence syndrome (NAS) NAS is characterized by increased irritability and signs of withdrawal, which are opposite to a hypo- reactive state.
Choice B rationale:
An excessive high-pitched cry is a hallmark sign of neonatal abstinence syndrome. Babies exposed to drugs like methadone during pregnancy can experience withdrawal symptoms, including a distinct high-pitched cry.
Choice C rationale:
Acrocyanosis, a bluish discoloration of the extremities, is a common finding in newborns and is not specific to NAS. It is caused by immature peripheral circulation and usually resolves on its own.
Choice D rationale:
A respiratory rate of 50/min is within the normal range for a newborn and is not a sign of neonatal abstinence syndrome. NAS symptoms are related to drug withdrawal and not respiratory issues.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
