A nurse is providing instructions to a newly licensed nurse about NG intubation for a client who is postoperative following a colectomy. Which of the following statements should the nurse include?
“Tube drainage should be rust-colored.”
“Nutrition will be provided through the tube.”
“The tube decreases pressure within the stomach.”
“The tube should be irrigated with sterile water.”
The Correct Answer is C
Choice A Reason
“Tube drainage should be rust-colored.” This statement is incorrect. Normal NG tube drainage is typically greenish-yellow due to bile or clear if it is from the stomach. Rust-colored drainage could indicate bleeding and should be reported immediately.
Choice B Reason
“Nutrition will be provided through the tube.” This statement is incorrect. While NG tubes can be used for feeding, in the context of a postoperative colectomy, the primary purpose of the NG tube is usually to decompress the stomach and prevent nausea and vomiting. Enteral feeding is typically done through a different type of tube, such as a nasojejunal tube.
Choice C Reason
“The tube decreases pressure within the stomach.” This is the correct statement. An NG tube is often used postoperatively to decompress the stomach, which helps to reduce pressure, prevent vomiting, and allow the gastrointestinal tract to heal.
Choice D Reason
“The tube should be irrigated with sterile water.” This statement is partially correct but needs context. NG tubes should be irrigated to maintain patency, but the type of solution (sterile water, saline) can vary based on hospital protocol. The primary focus here is on the purpose of the NG tube rather than the irrigation technique.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason
Place several pillows behind the client’s head. This intervention is incorrect. Placing several pillows behind the client’s head can lead to neck flexion, which can increase intracranial pressure by obstructing venous outflow from the brain.
Choice B Reason
Place the client in a lateral semi-prone recumbent position. This position is not ideal for managing increased intracranial pressure. The optimal position is to keep the head of the bed elevated at 30 degrees with the neck in a neutral position to promote venous drainage and reduce ICP.
Choice C Reason
Keep the client’s neck in a midline position. This is the correct intervention. Keeping the neck in a midline position helps to ensure proper venous drainage from the brain, thereby reducing intracranial pressure. It is a standard practice in managing patients with elevated ICP.
Choice D Reason
Maintain flexion of the client’s hips at a 90-degree angle. This intervention is incorrect. Flexion of the hips can increase intra-abdominal pressure, which in turn can increase intracranial pressure. It is important to avoid hip flexion in patients with elevated ICP.

Correct Answer is A
Explanation
Choice A Reason:
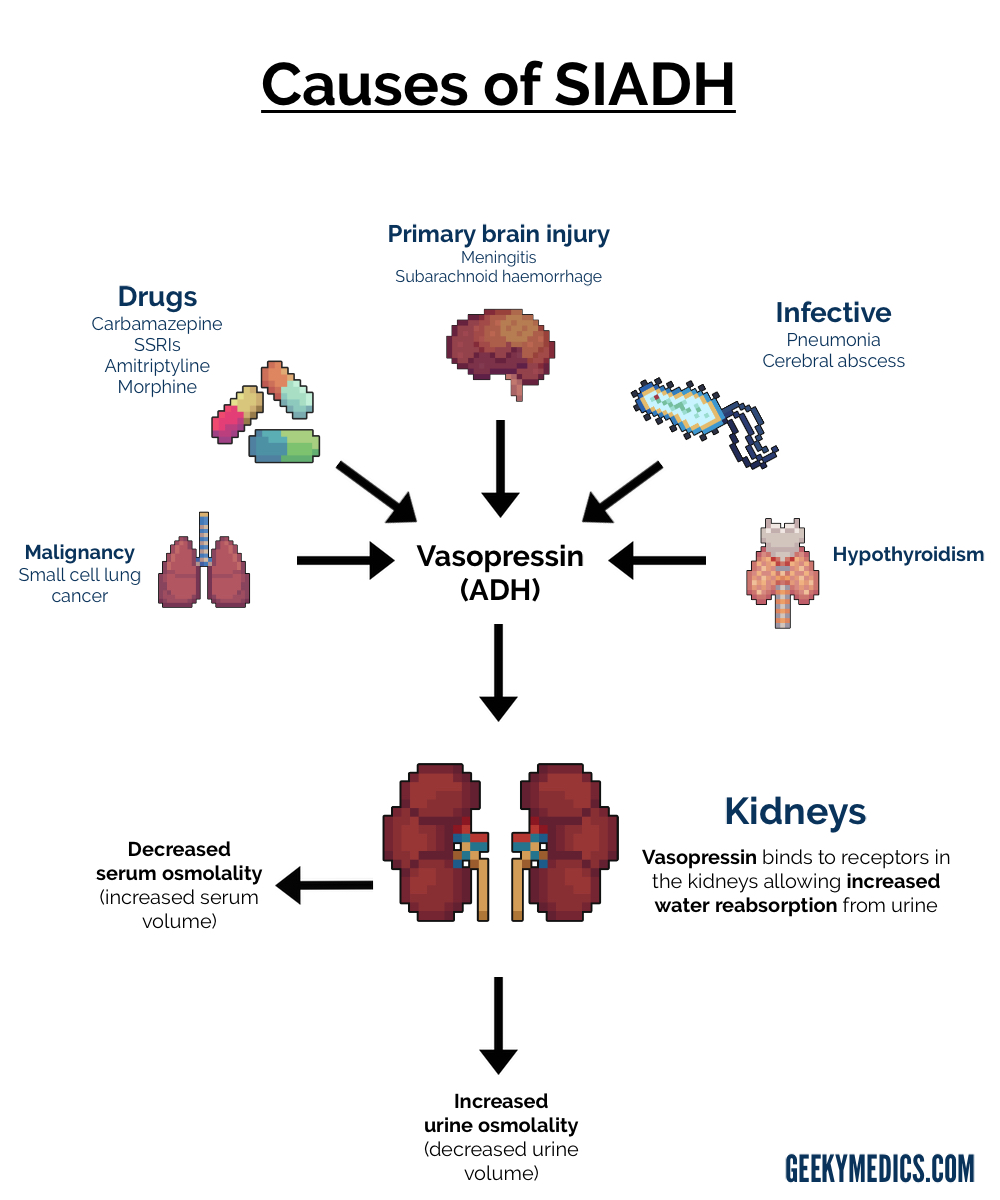
A urine specific gravity of 1.02 falls within the normal range (1.005 to 1.03) and indicates that the kidneys are excreting water appropriately. In SIADH, urine is typically concentrated due to excessive antidiuretic hormone (ADH) secretion. A normal urine specific gravity suggests that the ADH levels are normalizing and the condition is resolving.
Choice B Reason:
A sodium level of 119 mEq/L is significantly below the normal range (136 to 145 mEq/L) and indicates persistent hyponatremia. This finding suggests that the SIADH is not resolving, as effective treatment should lead to an increase in serum sodium levels.
Choice C Reason:
A BUN level of 8 mg/dL is slightly below the normal range (10 to 20 mg/dL) but is not a primary indicator of SIADH resolution. BUN levels can be influenced by various factors, including hydration status and renal function.
Choice D Reason:
A calcium level of 8.7 mg/dL is slightly below the normal range (9 to 10.5 mg/dL) but does not directly indicate the resolution of SIADH. Calcium levels are not typically used to monitor the effectiveness of SIADH treatment.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
