A nurse is providing teaching to a client with a colostomy about appropriate food choices. Which of the following foods should the nurse include in the teaching?
Dried fruits
Dried peas
Eggs
Pasta
The Correct Answer is C
Choice A reason: Dried fruits
Dried fruits are generally high in fiber, which can be problematic for individuals with a colostomy, especially in the initial weeks following surgery. High-fiber foods can increase stool bulk and may cause blockages or discomfort. It is recommended to avoid high-fiber foods until the digestive system has adjusted and the healthcare provider gives the go-ahead to reintroduce them gradually.
Choice B reason: Dried peas
Dried peas, like other legumes, are also high in fiber and can cause gas and bloating. These symptoms can be particularly uncomfortable for individuals with a colostomy. Additionally, legumes can increase the risk of blockages in the stoma. Therefore, it is advisable to avoid dried peas and other high-fiber legumes until the digestive system has fully adjusted.
Choice C reason: Eggs
Eggs are an excellent food choice for individuals with a colostomy. They are high in protein, which is essential for wound healing and overall recovery. Eggs are also easy to digest and do not typically cause gas or bloating. Including eggs in the diet can help ensure that the client receives adequate nutrition without causing digestive discomfort.
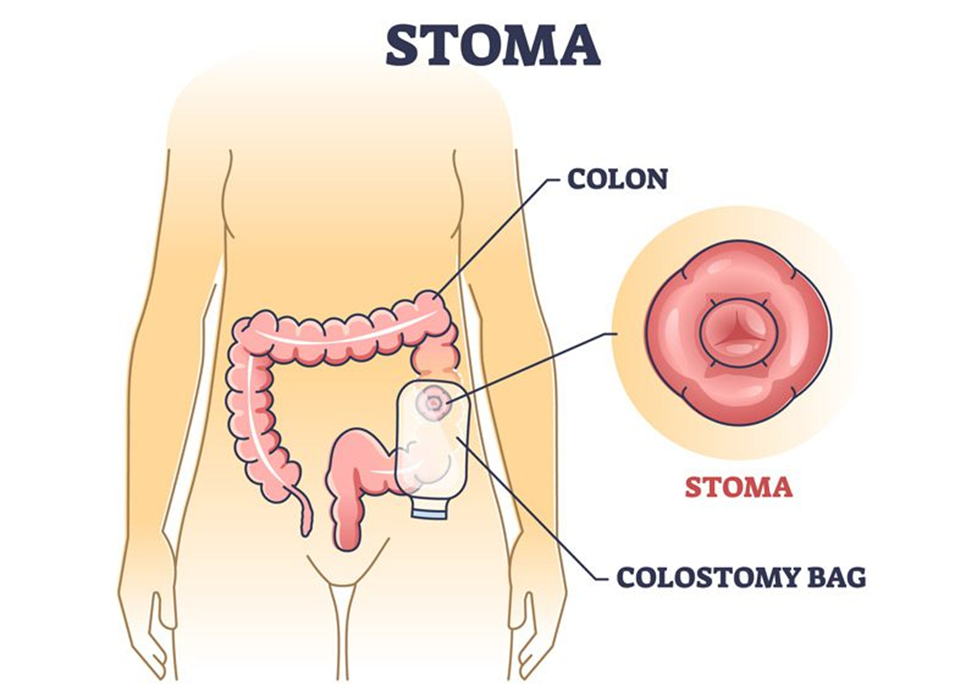
Choice D reason: Pasta
Pasta, particularly refined pasta, is generally low in fiber and easy to digest, making it a suitable food choice for individuals with a colostomy. It provides a good source of carbohydrates, which are important for energy. However, it is essential to monitor portion sizes and avoid adding high-fat or high-fiber ingredients that could cause digestive issues.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["B","C","D","E"]
Explanation
Choice A: Type and match for 2 units of packed RBCs
This option is not typically part of the initial management of sepsis. Typing and matching for blood transfusion is generally reserved for patients who are experiencing significant blood loss or severe anemia. In this case, the patient’s hemoglobin and hematocrit levels are within normal ranges, indicating that a blood transfusion is not immediately necessary. The primary focus in the first hour of sepsis management is to stabilize the patient through fluid resuscitation, infection control, and monitoring vital signs.
Choice B: Rapidly administer 30 mL/kg of normal saline
Rapid fluid resuscitation is a critical component of sepsis management. Administering 30 mL/kg of normal saline helps to restore intravascular volume, improve tissue perfusion, and prevent organ failure. This intervention is particularly important in patients with hypotension or elevated lactate levels, as it helps to maintain adequate blood pressure and oxygen delivery to tissues. The Surviving Sepsis Campaign guidelines recommend this approach to stabilize patients and prevent further complications.
Choice C: Measure lactate level
Measuring lactate levels is essential in the early management of sepsis. Elevated lactate levels indicate tissue hypoperfusion and anaerobic metabolism, which are hallmarks of sepsis and septic shock. Monitoring lactate levels helps to assess the severity of the condition and guide further treatment decisions. The Surviving Sepsis Campaign guidelines emphasize the importance of measuring lactate levels within the first hour of sepsis recognition. If the initial lactate level is elevated, it should be remeasured to evaluate the effectiveness of the interventions.
Choice D: Obtain blood cultures
Obtaining blood cultures before administering antibiotics is crucial for identifying the causative pathogen and tailoring antibiotic therapy. Blood cultures help to determine the source of infection and guide appropriate antimicrobial treatment. Early identification and targeted therapy are essential for improving patient outcomes in sepsis. The Surviving Sepsis Campaign guidelines recommend obtaining blood cultures as part of the initial management of sepsis.
Choice E: Obtain a wound culture
Obtaining a wound culture is important in this case because the patient has a wound with purulent drainage, which could be a potential source of infection. Identifying the specific pathogen responsible for the wound infection allows for targeted antibiotic therapy, which is more effective than broad-spectrum antibiotics. This intervention helps to control the source of infection and prevent further complications. The Surviving Sepsis Campaign guidelines support source control measures, including obtaining wound cultures, as part of the initial management of sepsis.
Correct Answer is B
Explanation
Choice A reason:
Turn the client every 4 hours: Regularly turning the client can help prevent pressure ulcers and improve overall circulation, but it is not the most effective measure specifically for preventing ventilator-associated pneumonia (VAP). While repositioning can help with lung expansion and secretion clearance, oral care is more directly related to reducing VAP risk.
Choice B reason:
Brush the client’s teeth with a suction toothbrush every 12 hours: Oral care is crucial in preventing VAP. Bacteria from the mouth can easily travel to the lungs, especially in intubated patients. Using a suction toothbrush helps remove dental plaque and secretions, reducing the bacterial load and the risk of infection. This practice is a key component of VAP prevention bundles.
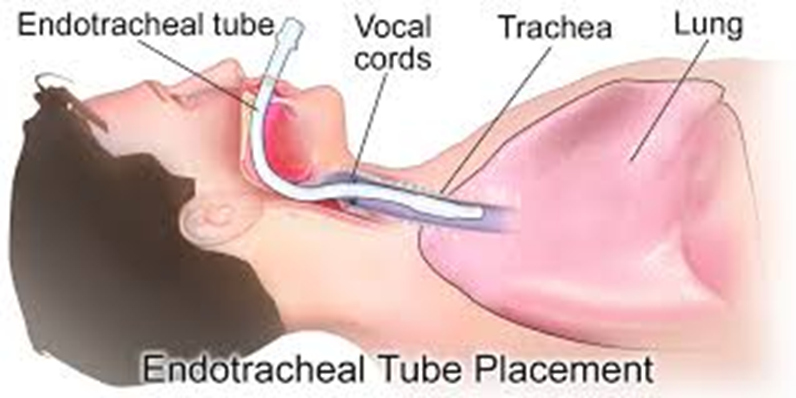
Choice C reason:
Provide humidity by maintaining moisture within the ventilator tubing: While maintaining humidity is important to prevent drying of the respiratory mucosa and to help with secretion clearance, it does not directly reduce the risk of VAP. Proper humidification is necessary for patient comfort and respiratory function but is not a primary VAP prevention strategy.
Choice D reason:
Position the head of the client’s bed in the flat position: Positioning the head of the bed flat can increase the risk of aspiration, which is a significant risk factor for VAP. The head of the bed should be elevated to 30-45 degrees to reduce the risk of aspiration and promote better lung expansion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
