A nurse is providing teaching to the parent of a newborn who has gastroesophageal reflux. Which of the following instructions should the nurse include?
Position the newborn at a 20-degree angle after feeding.
Dilute formula with 1 tablespoon of water.
Place the newborn in a side-lying position if vomiting.
Provide a small feeding just before bedtime.
The Correct Answer is A
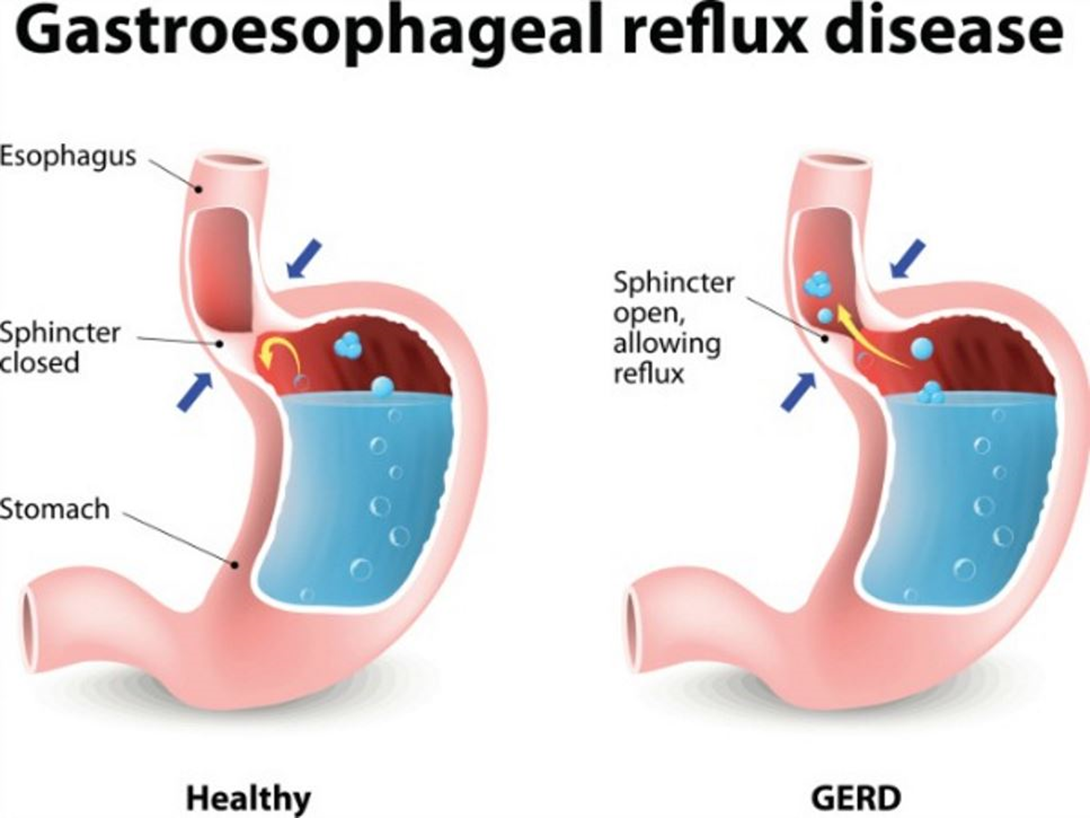
Choice A reason: Positioning the newborn at a 20-degree angle after feeding can help prevent the reflux of gastric contents into the esophagus. This position allows gravity to keep the food in the stomach and reduces the pressure on the lower esophageal sphincter. The nurse should instruct the parent to keep the newborn in this position for at least 30 minutes after each feeding.
Choice B reason: Diluting formula with 1 tablespoon of water is not recommended, as it can cause water intoxication, electrolyte imbalance, and malnutrition in the newborn. Water intoxication can lead to seizures, coma, and death. The nurse should advise the parent to follow the manufacturer's instructions for preparing the formula and not to add extra water.
Choice C reason: Placing the newborn in a side-lying position if vomiting is not a safe practice, as it can increase the risk of aspiration and sudden infant death syndrome (SIDS). Aspiration is when food or liquid enters the lungs and causes pneumonia or respiratory distress. SIDS is when a healthy baby dies suddenly and unexpectedly during sleep. The nurse should instruct the parent to place the newborn on the back for sleeping and to avoid soft bedding, pillows, and stuffed animals.
Choice D reason: Providing a small feeding just before bedtime is not a good idea, as it can worsen the gastroesophageal reflux and disrupt the newborn's sleep. The nurse should suggest the parent to feed the newborn smaller and more frequent meals throughout the day and to avoid feeding the newborn within 2 to 3 hours of bedtime.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice B reason: Older adults should decrease their calorie intake as their metabolic rate and physical activity tend to decline with age. Excess calories can lead to weight gain and increase the risk of chronic diseases such as diabetes, cardiovascular disease, and some cancers. Older adults should aim for a balanced diet that meets their nutritional needs without exceeding their energy requirements.
Choice A reason: Older adults should not decrease their vitamin D intake, as vitamin D is essential for bone health and immune function. Older adults are at risk of vitamin D deficiency due to reduced sun exposure, decreased skin synthesis, and impaired absorption. Vitamin D deficiency can cause osteoporosis, fractures, muscle weakness, and infections. Older adults should consume adequate amounts of vitamin D from fortified foods, supplements, or sun exposure.
Choice C reason: Older adults should not decrease their protein intake, as protein is important for maintaining muscle mass, strength, and function. Older adults are prone to sarcopenia, which is the loss of muscle mass and quality due to aging. Sarcopenia can impair mobility, balance, and independence. Older adults should consume enough protein from animal or plant sources to prevent or delay sarcopenia.
Choice D reason: Older adults should not decrease their fiber intake, as fiber is beneficial for digestive health and blood glucose control. Older adults often suffer from constipation, diverticular disease, and diabetes, which can be alleviated by increasing fiber intake. Fiber can also lower cholesterol levels and reduce the risk of heart disease and some cancers. Older adults should consume at least 25 grams of fiber per day from fruits, vegetables, whole grains, legumes, nuts, and seeds.
Correct Answer is D
Explanation
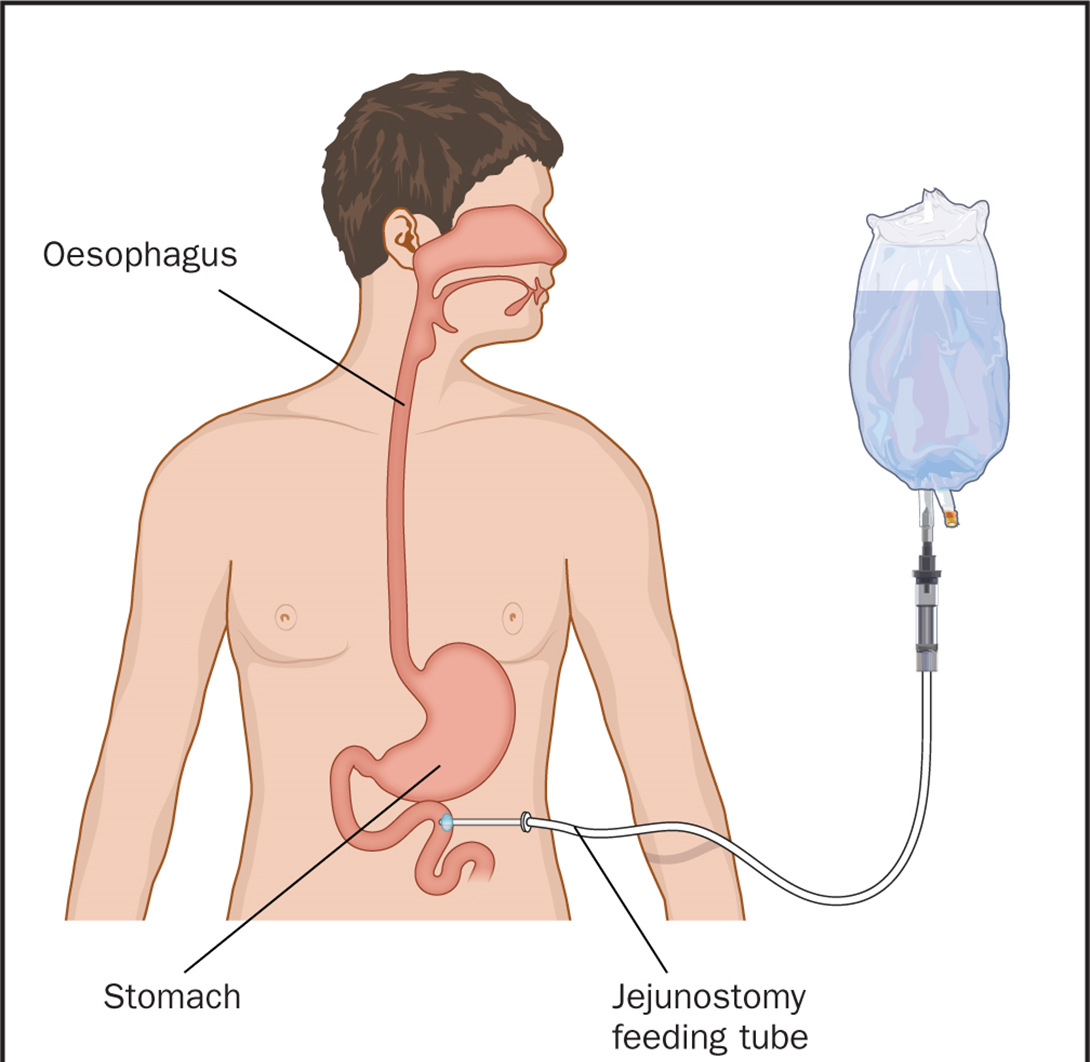
Choice A reason: Abdominal distention is a possible complication of enteral nutrition, as it may indicate gas accumulation, constipation, or intolerance to the formula. However, it is not the greatest risk to the client, as it can be prevented or managed by adjusting the formula, rate, or volume of the feeding, or by administering medications or enemas.
Choice B reason: Fluid overload is a possible complication of enteral nutrition, as it may indicate excessive fluid intake, renal impairment, or heart failure. However, it is not the greatest risk to the client, as it can be prevented or managed by monitoring the fluid balance, electrolytes, and vital signs, or by administering diuretics or fluid restriction.
Choice C reason: Glycosuria is a possible complication of enteral nutrition, as it may indicate hyperglycemia, diabetes, or infection. However, it is not the greatest risk to the client, as it can be prevented or managed by monitoring the blood glucose, urine output, and signs of infection, or by administering insulin or antibiotics.
Choice D reason: Tube obstruction is the greatest risk to the client, as it may indicate clogging, kinking, or twisting of the tube, which can impair the delivery of the nutrition and medication, and cause aspiration, infection, or perforation. Tube obstruction can be prevented by flushing the tube with water before and after each feeding or medication, and by using a syringe or a pump to administer the formula. Tube obstruction can be managed by using warm water, carbonated beverages, or pancreatic enzymes to unclog the tube, or by replacing the tube if necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
