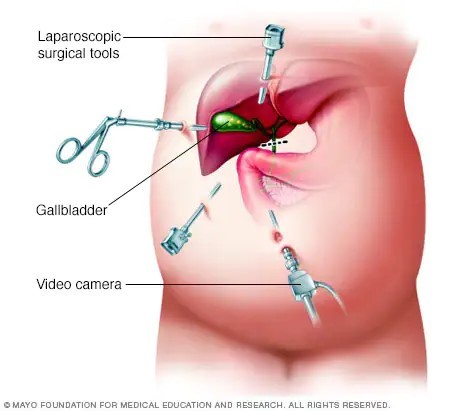
A nurse is reinforcing teaching with a client who is postoperative following a laparoscopic cholecystectomy. Which of the following statements by the client indicates an understanding of the teaching?
“I should eat a high-fat diet for several weeks."
"I should expect to have diarrhea until my diet changes."
"I should expect to have nausea for several days."
"I should leave my steri-strips on until they fall off."
The Correct Answer is D
After a laparoscopic cholecystectomy, steri-strips or adhesive strips are commonly placed over the small incisions. The client should keep the steri-strips in place until they fall off on their own or until they are removed by the healthcare provider during a follow-up visit. Removing the steri-strips prematurely can increase the risk of infection or disrupt the healing process.
"I should eat a high-fat diet for several weeks": After a laparoscopic cholecystectomy, it is important for the client to follow a low-fat diet initially to allow the body time to adjust to the absence of the gallbladder. High-fat foods can be more difficult to digest and may cause digestive discomfort. Gradually introducing small amounts of fat back into the diet is recommended, but a high-fat diet is not appropriate.
"I should expect to have diarrhea until my diet changes": While changes in bowel movements can occur after a cholecystectomy, such as looser stools or changes in frequency, persistent diarrhea is not expected or normal. If the client experiences persistent diarrhea, they should contact their healthcare provider for further evaluation.
"I should expect to have nausea for several days": While some clients may experience mild nausea or discomfort after the surgery, it should generally improve within a few days. If the client experiences persistent or severe nausea, they should contact their healthcare provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Furosemide works by promoting diuresis, which helps to reduce fluid volume overload in heart failure. Increased urinary output indicates that the medication is effectively removing excess fluid from the body. This can help alleviate symptoms such as edema and fluid retention commonly associated with heart failure. Therefore, an increased urinary output is a positive response to furosemide therapy in this context.
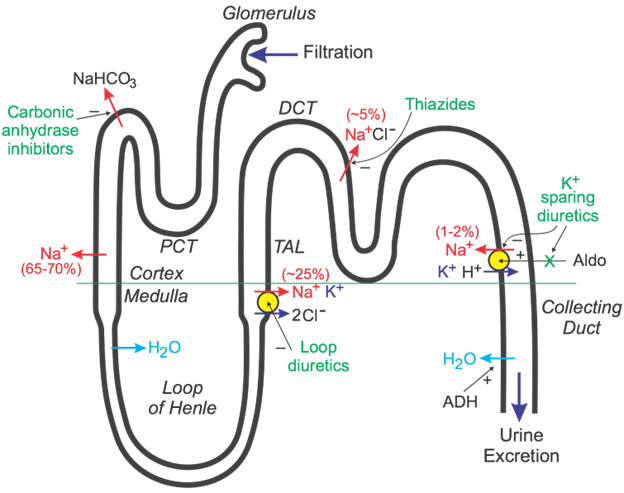
Decreased BUN (blood urea nitrogen) levels and weight loss are also expected outcomes of diuretic therapy, further indicating the effectiveness of the medication. However, a decreased hemoglobin level is not directly related to the efficacy of furosemide and might be indicative of other factors such as anemia or bleeding, requiring further assessment and intervention.
Correct Answer is ["A","B","D"]
Explanation
The nurse should take the following actions when receiving a telephone prescription from a client's provider:
- Ask the provider to spell out the name of the medication: This is important to ensure accurate transcription of the medication name. Spelling out the name helps prevent errors due to similar-sounding medications or confusion with abbreviations.
- Request that the provider confirm the read-back of the prescription: This step ensures that the nurse and the provider are on the same page and that the prescription has been accurately transcribed. It allows for verification and correction if any discrepancies are identified.
- Record the date and time of the telephone prescription: Documenting the date and time of the telephone prescription is essential for tracking and reference purposes. It helps establish a clear timeline of events and ensures proper documentation of the medication order.
It is not necessary to withhold the medication until the provider signs the prescription, as telephone prescriptions are typically followed up with a written prescription or electronic verification.
Instructing another nurse to record the prescription in the medical record may not be necessary, as the nurse who received the telephone prescription is responsible for accurately documenting the order in the medical record. However, if necessary, the nurse can delegate the task of documentation to another qualified staff member under their supervision, ensuring accuracy and completeness.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
