A nurse is reviewing blood glucose values for a client who is at risk for diabetes mellitus. Which of the following findings should the nurse report to the provider?
Fasting blood glucose 70 mg/dL
2-hr glucose tolerance test level 150 mg/dL
Glycosylated hemoglobin 5%
Casual blood glucose 90 mg/dL
The Correct Answer is B
2-hour glucose tolerance test level 150 mg/dL: The 2-hour glucose tolerance test level of 150 mg/dL indicates elevated blood glucose levels after a glucose challenge. This finding suggests impaired glucose tolerance or impaired fasting glucose, which are considered pre-diabetic states. It is important to report this finding to the provider for further evaluation and consideration of interventions to prevent or delay the development of diabetes mellitus.
Fasting blood glucose 70 mg/dL: A fasting blood glucose level of 70 mg/dL is within the normal range. Typically, fasting blood glucose levels below 100 mg/dL are considered normal.
Therefore, this finding does not indicate a concern for diabetes.
Glycosylated hemoglobin 5%: A glycosylated hemoglobin (HbA1c) level of 5% is within the normal range. HbA1c is a measure of average blood glucose levels over the past two to three months, and a level below 5.7% is typically considered normal. Therefore, this finding does not indicate a concern for diabetes.
Casual blood glucose 90 mg/dL: A casual blood glucose level of 90 mg/dL is within the normal range. Casual blood glucose levels below 140 mg/dL are generally considered normal.
Therefore, this finding does not indicate a concern for diabetes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Administer antiemetics on a schedule. Antiemetics are medications used to prevent or relieve nausea and vomiting. By administering them on a schedule, the nurse can help manage and control the client's nausea more effectively.
Providing a snack 30 minutes before treatments is not an appropriate intervention for nausea associated with radiation therapy. In fact, eating before radiation therapy may worsen nausea in some individuals. It is generally recommended to have a light meal or snack a few hours before the treatment to avoid an empty stomach but also prevent overeating that can trigger nausea.
Ensuring foods are served hot is not a recommended intervention for nausea. In fact, hot foods may exacerbate nausea in some individuals. It is advisable to serve foods at a cooler or room temperature, as cooler foods may be better tolerated.
Serving low carbohydrate meals is not specific to managing nausea associated with radiation therapy. While some individuals may find low carbohydrate meals easier to digest, there is no strong evidence suggesting that they alleviate nausea specifically. The choice of meals should be based on the client's preferences, tolerance, and any dietary restrictions they may have.
Correct Answer is A
Explanation
Celiac disease is an autoimmune disorder in which the ingestion of gluten, a protein found in wheat, rye, and barley, triggers an immune response and causes damage to the small intestine. Therefore, individuals with celiac disease need to follow a strict gluten-free diet.
Rice cereal with sliced bananas: This is a suitable choice as long as the rice cereal is gluten-free and there is no cross-contamination with gluten-containing ingredients. Rice is
naturally gluten-free, and fresh fruits like bananas are safe for individuals with celiac disease.
Rye toast with herbal tea: Rye is a gluten-containing grain, so rye toast is not suitable for someone with celiac disease. Herbal tea is typically gluten-free, but the toast is not appropriate.
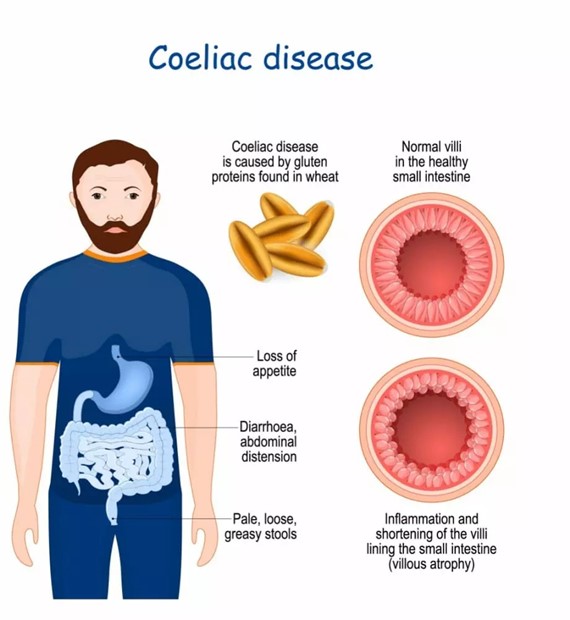
Graham crackers with peanut butter: Graham crackers are usually made with wheat flour, which contains gluten. Therefore, they are not suitable for someone with celiac disease.
Poached eggs with wheat bagel: Wheat is a gluten-containing grain, so a wheat bagel is not appropriate for someone with celiac disease.
It is essential for individuals with celiac disease to carefully read food labels and select gluten-free options.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
