A nurse is reviewing the laboratory results of a client who is at 32 weeks of gestation and has preeclampsia. The nurse should identify that which of the following findings is indicated with HELLP syndrome?
Bilirubin 1 mg/dL (0.1 to 1 mg/dL)
Uric acid 6.8 mg/dL (2 to 6.6 mg/dL)
Fibrinogen 500 mg/dL (200 to 400 mg/dL)
Aspartate aminotransferase 80 units/L (4 to 20 units/L)
The Correct Answer is D
A. Bilirubin 1 mg/dL (0.1 to 1 mg/dL):
Bilirubin levels can be elevated in conditions involving liver dysfunction or hemolysis, such as HELLP syndrome. However, a bilirubin level of 1 mg/dL falls within the normal range (0.1 to 1 mg/dL). While bilirubin levels may be elevated in some cases of HELLP syndrome, this particular value is not indicative of HELLP syndrome.
B. Uric acid 6.8 mg/dL (2 to 6.6 mg/dL):
Elevated uric acid levels are commonly seen in preeclampsia, but they are not specific to HELLP syndrome. Uric acid levels can rise due to decreased renal function and increased cell breakdown. However, while a level of 6.8 mg/dL is slightly elevated compared to the normal range (2 to 6.6 mg/dL), it alone does not confirm the presence of HELLP syndrome.
C. Fibrinogen 500 mg/dL (200 to 400 mg/dL):
Fibrinogen levels are typically increased in pregnancy, but they can be decreased in conditions associated with consumption coagulopathy, such as disseminated intravascular coagulation (DIC). However, elevated fibrinogen levels are not typically associated with HELLP syndrome. A level of 500 mg/dL is above the normal range (200 to 400 mg/dL), but this finding alone does not indicate HELLP syndrome.
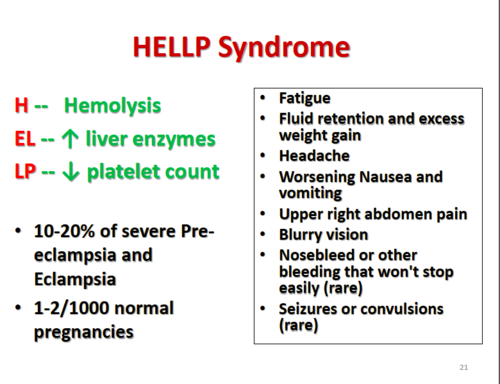
D. Aspartate aminotransferase (AST) 80 units/L (4 to 20 units/L):
Aspartate aminotransferase (AST) is a liver enzyme that can be elevated in liver injury or dysfunction, which can occur in HELLP syndrome. An AST level of 80 units/L is significantly elevated compared to the normal range (4 to 20 units/L), suggesting liver dysfunction. Elevated liver enzymes are a characteristic feature of HELLP syndrome, making this finding the most indicative of HELLP syndrome among the options provided.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","D","G"]
Explanation
A. Uterine tone soft:A soft uterus can indicate inadequate uterine contraction, which may increase the risk of postpartum hemorrhage. The uterus should be firm and well-contracted after delivery.
B. Blood pressure 136/86 mm Hg:
A blood pressure of 136/86 mm Hg is within the normal range for a postpartum client. While changes in blood pressure should be monitored, this reading alone does not indicate an urgent need for follow-up.
C. Peripheral edema 2+ bilateral lower extremities:
Peripheral edema is a common finding in the postpartum period and is often attributed to fluid shifts and hormonal changes. While it should be monitored, it does not typically require immediate follow-up unless it is severe or associated with other symptoms.
D. Large amount of lochia rubra: While lochia rubra is normal in the first few days postpartum, a large amount could indicate potential bleeding issues or complications if it increases significantly.
E. Pain rating of 3 on a scale of 0 to 10:
A pain rating of 3 on a scale of 0 to 10 is relatively mild and may be expected after a vaginal delivery, especially if the client has undergone an episiotomy. It should be addressed but does not require immediate follow-up unless it worsens or is associated with other concerning symptoms.
F. Breasts soft:
Soft breasts are expected in the early postpartum period, particularly if the client is not breastfeeding or if breastfeeding has not yet been established. However, breastfeeding assessment and support should be provided as part of routine postpartum care.
G. Lateral deviation of the uterus:The uterus should be midline and firm. A lateral deviation could suggest a full bladder or other complications that need to be addressed to prevent further issues such as postpartum hemorrhage.
H. Deep tendon reflexes 1+:
Deep tendon reflexes of 1+ are within the normal range and do not typically require immediate follow-up unless they are absent or hyperactive, which may indicate neurological issues.
Correct Answer is {"A":{"answers":"C"},"B":{"answers":"A"},"C":{"answers":"B"},"D":{"answers":"B"}}
No explanation
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
