A nurse is teaching a class about physiological changes to hearing in older adult clients. Which of the following should the nurse include?
Decreased thickness of tympanic membranes
Decreased tinnitus
Decreased ear wax
Decreased ability to hear high-frequency sounds
The Correct Answer is D
Choice A Reason: Decreased thickness of tympanic membranes is not a physiological change to hearing in older adult clients. The tympanic membranes are thin and flexible structures that vibrate in response to sound waves. The thickness of the tympanic membranes does not change significantly with age.
Choice B Reason: Decreased tinnitus is not a physiological change to hearing in older adult clients. Tinnitus is a ringing or buzzing sound in the ears that may be caused by various factors, such as noise exposure, ear infections, medications, or aging. Tinnitus may increase or decrease with age, depending on the underlying cause.
Choice C Reason: Decreased ear wax is not a physiological change to hearing in older adult clients. Ear wax is a natural substance that lubricates and protects the ear canal from dust, bacteria, and insects. Ear wax production may vary with age, but it does not affect hearing unless it accumulates and blocks the ear canal.
Choice D Reason: Decreased ability to hear high-frequency sounds is a physiological change to hearing in older adult clients. This is also known as presbycusis, which is a gradual loss of hearing that occurs as part of aging. Presbycusis affects the ability to hear high-pitched sounds, such as consonants, birdsong, or alarms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["D","E"]
Explanation
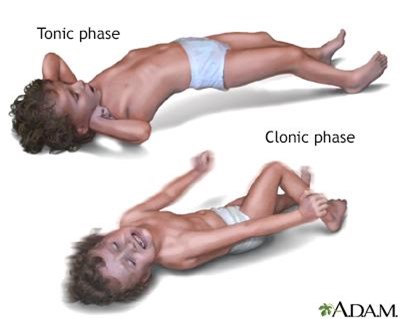
Choice A Reason: This choice is incorrect. Placing the client into a supine position is not an action that the nurse should take, as it can compromise the airway and increase the risk of aspiration. The nurse should position the client on their side with their head tilted slightly forward to allow saliva and secretions to drain out of their mouth.
Choice B Reason: This choice is incorrect. Applying restraints is not an action that the nurse should take, as it can cause injury and increase agitation. The nurse should protect the client from harm by removing any objects or furniture that may cause harm and padding any hard surfaces with blankets or pillows.
Choice C Reason: This choice is incorrect. Inserting a bite stick into the client's mouth is not an action that the nurse should take, as it can cause injury and obstruction. The nurse should never force anything into the client's mouth during a seizure, as it can damage their teeth, gums, tongue, or jaw.
Choice D Reason: This is a correct choice. Loosening restrictive clothing is an action that the nurse should take, as it can improve breathing and circulation. The nurse should unbutton any tight collars, belts, or ties that may constrict the chest or neck.
Choice E Reason: This is a correct choice. Placing a pillow under the client's head is an action that the nurse should take, as it can prevent injury and provide comfort. The nurse should support the client's head with a soft pillow or cushion to prevent hitting it against any hard surfaces.
Correct Answer is D
Explanation
Choice A reason: This is incorrect because this comment does not require reporting to the client's provider. It is normal to have reduced vision and an increased risk of falling with a patch on one eye after cataract surgery. The nurse should reassure the client, provide assistance with mobility, and educate the client on safety measures.
Choice B reason: This is incorrect because this comment does not require reporting to the client's provider. It is normal to have some itching and discomfort in the eye after cataract surgery. The nurse should commend the client for not rubbing the eye, as this can cause infection or damage to the surgical site. The nurse should also administer anti-inflammatory eye drops as prescribed and instruct the client on how to apply them.
Choice C reason: This is incorrect because this comment does not require reporting to the client's provider. It is normal to have increased sensitivity to light in the eye after cataract surgery. The nurse should dim the lights in the room, provide sunglasses or a shield for the eye, and educate the client on how to protect the eye from bright light.
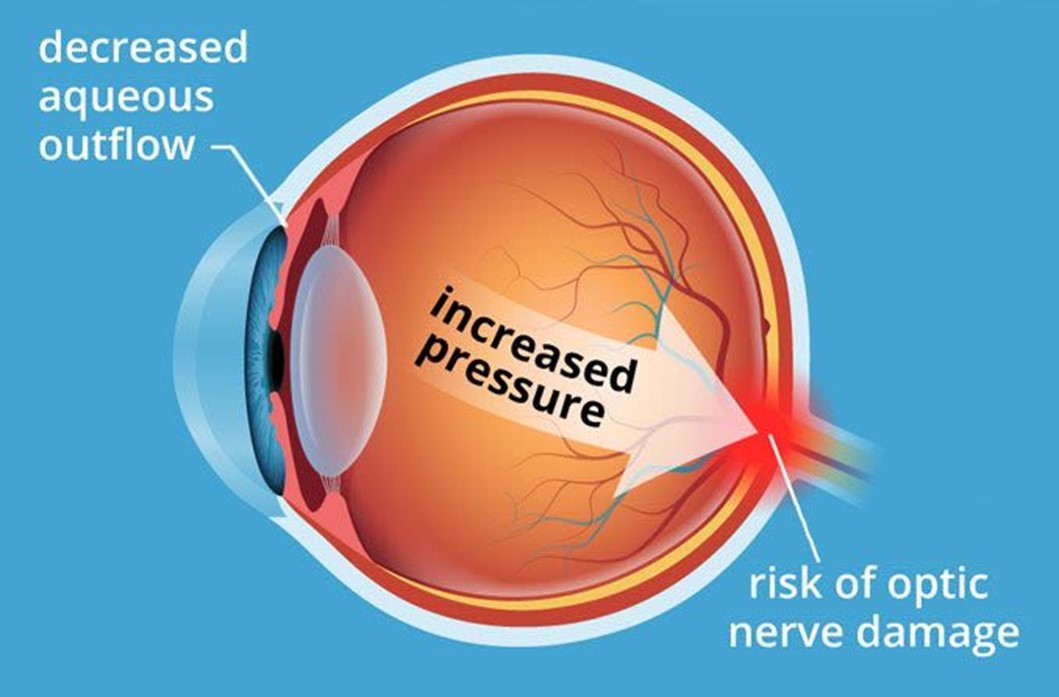
Choice D reason: This is the correct answer because this comment requires reporting to the client's provider. Severe pain in the eye after cataract surgery can indicate a complication such as infection, inflammation, bleeding, or increased intraocular pressure. The nurse should assess the eye for signs of redness, swelling, discharge, or bleeding, and report the findings and the pain level to the provider. The nurse should also administer analgesics as prescribed and monitor the pain relief.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
