A nurse working in an emergency department is performing triage. To which of the following clients should the nurse assign priority?
A client who reports night sweats and fever for the last week
A client who has compound fractures of the tibia and humerus
A client who reports severe vomiting and diarrhea
A client who has soot markings around each naris following a house fire
The Correct Answer is D
a. A client who reports night sweats and fever for the last week:
Night sweats and fever can be indicative of various underlying conditions, including infections. While these symptoms may require medical attention, they do not necessarily indicate an immediately life-threatening condition compared to other options.
b. A client who has compound fractures of the tibia and humerus:
Compound fractures involve broken bones that penetrate through the skin, leading to a risk of severe bleeding, infection, and other complications. This client's injuries are significant and require immediate attention to prevent further complications and provide pain management and stabilization.
c. A client who reports severe vomiting and diarrhea:
Severe vomiting and diarrhea can lead to dehydration, electrolyte imbalances, and other complications, especially if prolonged or accompanied by other symptoms such as fever. While this client requires prompt assessment and treatment, the urgency may not be as high as for other conditions.
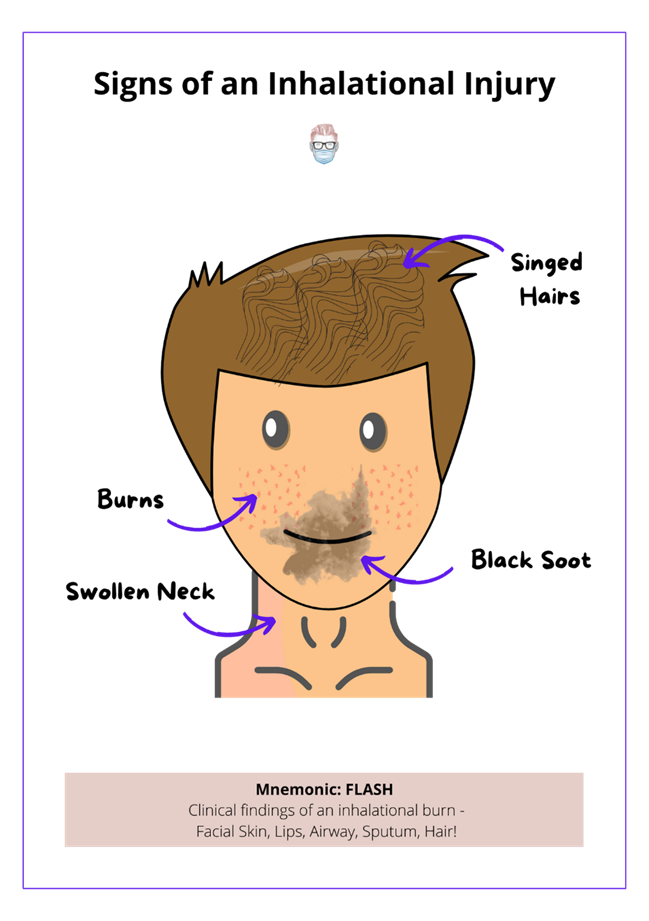
d. A client who has soot markings around each naris following a house fire:
Soot markings around the nares (nostrils) suggest inhalation injury, which can lead to airway compromise, respiratory distress, and other serious complications. This client requires immediate assessment and intervention to ensure airway patency, oxygenation, and respiratory support.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
a. Is the client’s family present so the AP can show them how to turn the client:
While involving the client's family in care can be beneficial for education and support, this assessment does not directly pertain to the AP's ability to provide care or the client's immediate needs.
b. Does the AP have time to change the client’s central IV-line dressing after turning her:
This assessment is relevant to the AP's workload and scheduling, but it does not directly address the client's care needs related to bathing and turning.
c. Has data been collected about specific client needs related to turning:
This assessment is crucial before delegating care. The nurse should ensure that relevant information about the client's condition, including any specific needs or considerations related to turning, has been gathered and communicated to the AP to provide appropriate care.
d. Has the AP checked the client’s pain level prior to turning her:
This assessment is essential to ensure the client's comfort and safety during care activities. Assessing the client's pain level before turning helps prevent exacerbation of pain and ensures that turning is performed with appropriate consideration for the client's comfort.
Correct Answer is B
Explanation
a. Recommend the AP come back later when the record is available:
This option delays the documentation process unnecessarily and may inconvenience the AP.
It doesn't address the issue of maintaining patient confidentiality and accurate documentation.
b. Log out so the AP can log in to document the vital signs:
This is the correct choice as it ensures that each individual's documentation is attributed to the correct user.
It maintains patient confidentiality and adheres to HIPAA regulations.
It allows the AP to complete their task efficiently while preserving the integrity of the electronic record.
c. Offer to chart the vital signs for the AP:
This option involves the nurse taking over the responsibility of documenting the vital signs for the AP, which could lead to confusion and potential errors.
It's not the most appropriate solution as it may not be feasible for the nurse to document the vital signs accurately without directly measuring them.
d. Allow the AP to document the vital signs prior to logging out:
Allowing the AP to document vital signs under the nurse's login compromises the integrity of the electronic record and violates HIPAA regulations.
It's not an acceptable practice as it can lead to inaccuracies in the documentation and compromises patient confidentiality.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
