A patient presents with a retinal detachment and is being evaluated for appropriate treatment. Which of the following procedures is used to treat retinal detachment by indenting the wall of the eye?
Scleral buckling
Photorefractive keratectomy (PRK)
Vitrectomy
Intravitreal injection
The Correct Answer is A
Choice A Reason:
Scleral buckling is a surgical procedure used to treat retinal detachment by indenting the wall of the eye. This technique involves placing a silicone band (buckle) around the sclera (the white part of the eye) to push the wall of the eye against the detached retina. This helps to reattach the retina and prevent further detachment. Scleral buckling is effective in treating many types of retinal detachments and is a common procedure for this condition.
Choice B Reason:
Photorefractive keratectomy (PRK) is a type of refractive surgery used to correct vision problems such as myopia, hyperopia, and astigmatism. It involves reshaping the cornea using a laser but is not used to treat retinal detachment. PRK does not involve indenting the wall of the eye or addressing issues with the retina.
Choice C Reason:
Vitrectomy is a surgical procedure that involves removing the vitreous gel from the eye to treat various eye conditions, including retinal detachment. While vitrectomy can be used to treat retinal detachment, it does not involve indenting the wall of the eye. Instead, it allows the surgeon to access the retina and perform necessary repairs.
Choice D Reason:
Intravitreal injection involves injecting medication directly into the vitreous cavity of the eye. This procedure is used to treat conditions such as macular degeneration, diabetic retinopathy, and retinal vein occlusion. It is not used to treat retinal detachment by indenting the wall of the eye.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
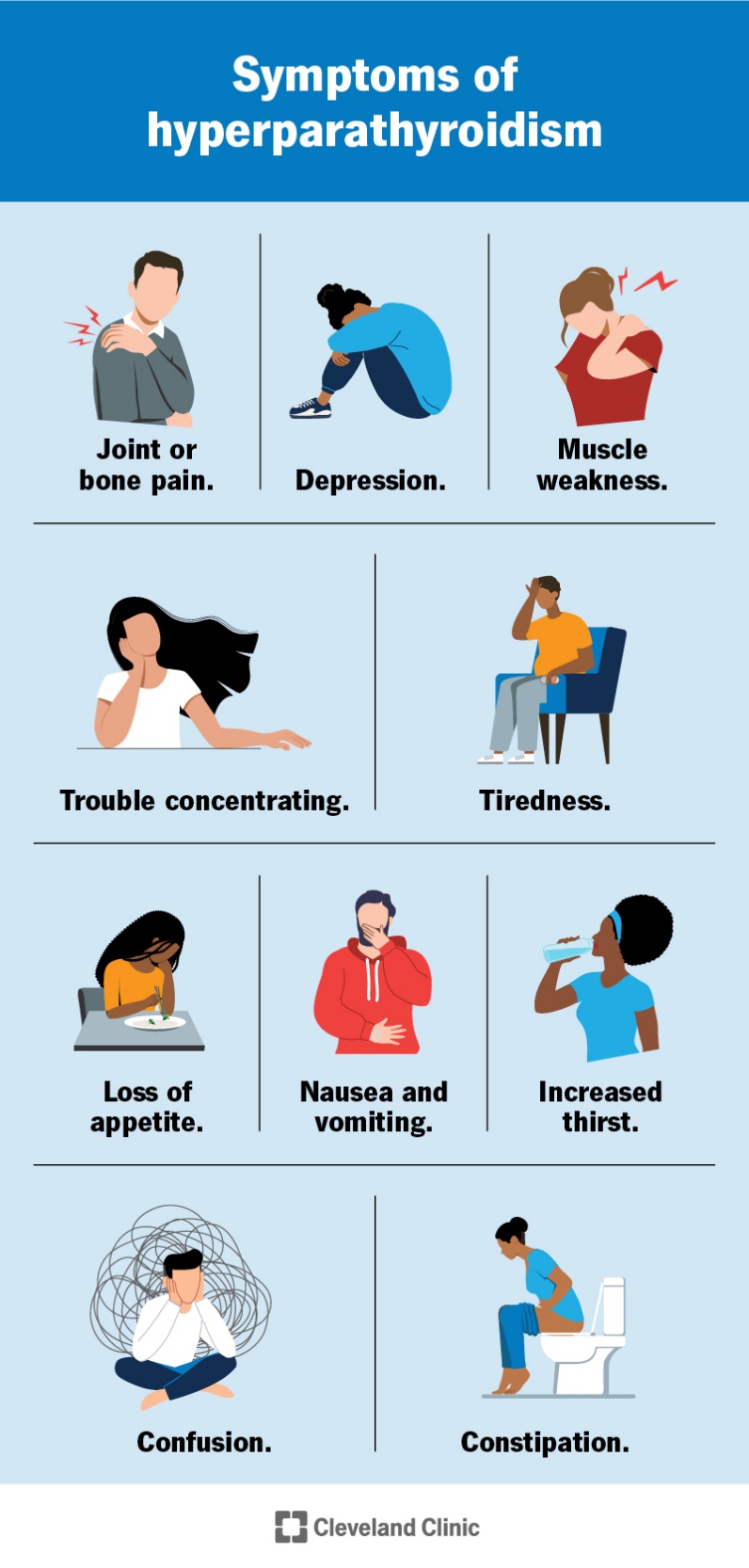
An adenoma of the parathyroid gland is the most common cause of primary hyperparathyroidism. This benign tumor leads to the overproduction of parathyroid hormone (PTH), which in turn causes elevated calcium levels in the blood. The excessive PTH secretion disrupts the normal calcium balance, leading to symptoms such as fatigue, muscle weakness, and depression. Parathyroid adenomas account for approximately 80% of primary hyperparathyroidism cases.
Choice B Reason:
Thyroid carcinoma is a type of cancer that originates in the thyroid gland, not the parathyroid glands. While thyroid carcinoma can cause various symptoms, it does not typically lead to elevated PTH levels or hyperparathyroidism. Therefore, it is not the most likely cause of the patient’s condition.
Choice C Reason:
Vitamin D deficiency can lead to secondary hyperparathyroidism, where low levels of vitamin D cause decreased calcium absorption, prompting the parathyroid glands to produce more PTH to maintain calcium levels. However, this condition is usually associated with low or normal calcium levels, not elevated calcium levels as seen in this patient. Therefore, it is not the most likely cause of her hyperparathyroidism.
Choice D Reason:
Chronic kidney disease (CKD) can also cause secondary hyperparathyroidism due to impaired kidney function, which affects calcium and phosphate balance and vitamin D metabolism. However, similar to vitamin D deficiency, CKD-related hyperparathyroidism typically presents with low or normal calcium levels rather than elevated levels. Thus, it is not the most likely cause in this scenario.
Correct Answer is A
Explanation
Choice A Reason:
Administering IV levothyroxine is the priority intervention for a patient with myxedema coma. Myxedema coma is a severe form of hypothyroidism that requires immediate thyroid hormone replacement to correct the deficiency and stabilize the patient’s condition. Intravenous levothyroxine is preferred because it provides a rapid increase in thyroid hormone levels, which is crucial for reversing the life-threatening symptoms of myxedema coma, such as hypothermia, bradycardia, and altered mental status.
Choice B Reason:
Starting broad-spectrum antibiotics is not the primary intervention for myxedema coma. While infections can precipitate myxedema coma and should be treated if present, the immediate priority is to address the severe hypothyroidism with thyroid hormone replacement. Antibiotics may be administered if an infection is suspected or confirmed, but they do not directly address the underlying thyroid hormone deficiency.
Choice C Reason:
Administering corticosteroids immediately is important but not the highest priority. Corticosteroids are often given to patients with myxedema coma to treat potential adrenal insufficiency, which can coexist with severe hypothyroidism. However, the primary intervention remains the administration of thyroid hormone replacement to correct the hypothyroid state.
Choice D Reason:
Initiating fluid restriction is not appropriate for managing myxedema coma. Patients with myxedema coma often require careful fluid management to address potential hyponatremia and maintain hemodynamic stability. Fluid restriction is not a standard intervention for this condition and does not address the critical need for thyroid hormone replacement.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
