A 55-year-old patient is diagnosed with Meniere’s disease. Which of the following symptoms is most characteristic of this condition?
Shortness of breath.
Chest pain.
Fever.
Vertigo.
The Correct Answer is D
Choice A Reason:
Shortness of breath is not typically associated with Meniere’s disease. This condition primarily affects the inner ear, leading to symptoms related to balance and hearing. Shortness of breath is more commonly linked to respiratory or cardiovascular issues.
Choice B Reason:
Chest pain is not a characteristic symptom of Meniere’s disease. Chest pain is usually related to cardiac or musculoskeletal problems. Meniere’s disease affects the inner ear and does not typically cause chest pain.
Choice C Reason:
Fever is not a common symptom of Meniere’s disease. Fever is generally associated with infections or inflammatory conditions. Meniere’s disease involves the buildup of fluid in the inner ear, leading to vertigo, tinnitus, and hearing loss, but not fever.
Choice D Reason:
Vertigo is the most characteristic symptom of Meniere’s disease. Vertigo involves a spinning sensation that can be severe and debilitating. It is caused by the abnormal fluid buildup in the inner ear, which disrupts the balance and hearing functions. This symptom is a hallmark of Meniere’s disease and is often accompanied by tinnitus and hearing loss.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
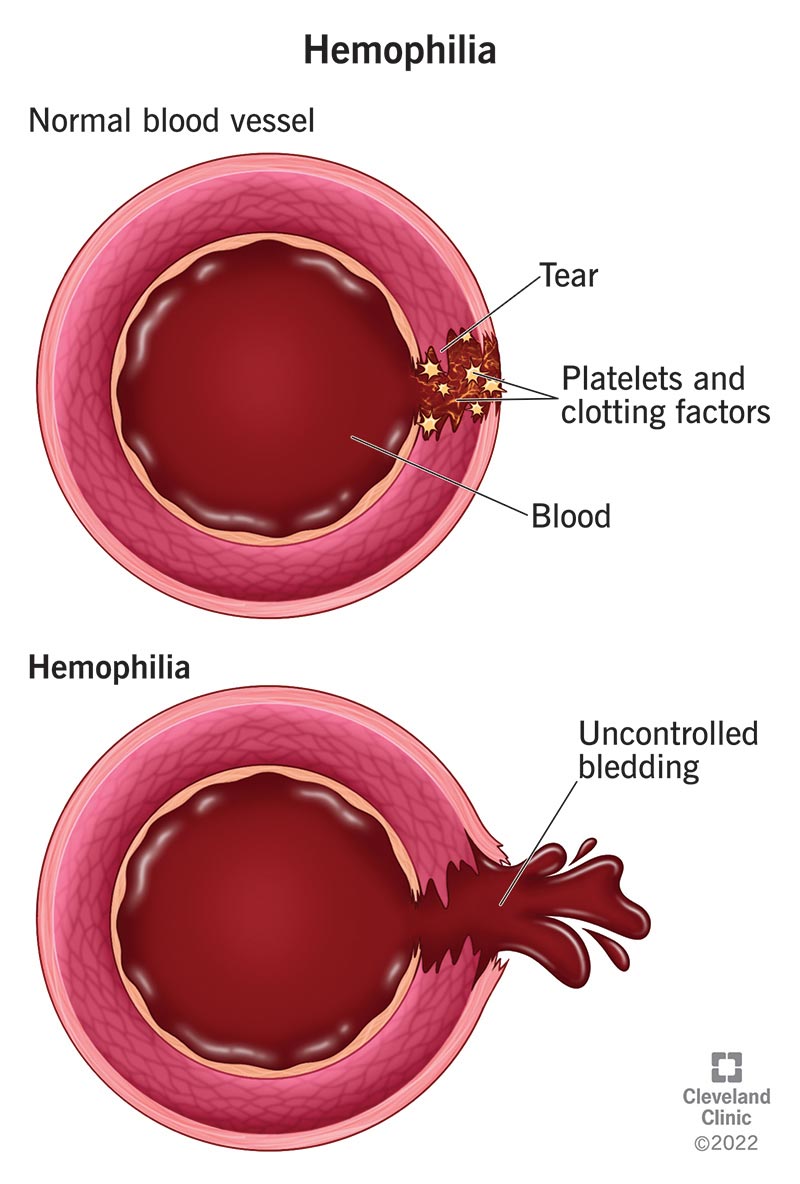
Preparing the patient for immediate surgical intervention is not the first-line treatment for hemophilia-related joint bleeding. Surgery is considered only if there is severe damage or if conservative measures fail. Initial management focuses on controlling bleeding and reducing inflammation.
Choice B Reason:
Administering aspirin for pain relief is contraindicated in patients with hemophilia. Aspirin inhibits platelet function and can exacerbate bleeding. Alternative pain management strategies that do not affect clotting should be used.
Choice C Reason:
Applying ice to the affected knee and elevating the leg is the most appropriate initial intervention. Ice helps to reduce swelling and pain, while elevation minimizes blood flow to the area, helping to control bleeding. This conservative approach is crucial in managing acute hemarthrosis in hemophilia patients.
Choice D Reason:
Performing passive range of motion exercises on the affected knee is not recommended during the acute phase of hemarthrosis. Movement can increase bleeding and worsen the condition. Rest and immobilization are preferred until the bleeding is controlled.
Correct Answer is A
Explanation
Choice A Reason:
Stopping the transfusion immediately and notifying the healthcare provider is the most appropriate initial action when a transfusion reaction is suspected. This action helps to prevent further complications and allows for prompt evaluation and management of the reaction. The nurse should also keep the IV line open with normal saline to maintain venous access.
Choice B Reason:
Administering antipyretics and continuing the transfusion is not appropriate. Continuing the transfusion could exacerbate the reaction and lead to more severe complications. The priority is to stop the transfusion and assess the patient before considering any further interventions.
Choice C Reason:
Slowing down the rate of the transfusion and reassessing in 30 minutes is not a safe approach. Any signs of a transfusion reaction, such as chills and fever, require immediate cessation of the transfusion. Delaying intervention could result in worsening of the patient’s condition.
Choice D Reason:
Continuing the transfusion and monitoring the patient closely is not appropriate. Immediate cessation of the transfusion is necessary to prevent further exposure to the potentially harmful blood product. Monitoring alone is insufficient without stopping the transfusion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
