An 18-year-old patient with a known history of sickle cell anemia presents to the emergency department with severe pain in the lower back and joints, fever, and signs of dehydration. What is the most appropriate initial nursing intervention?
Administer intravenous fluids and pain management as prescribed.
Apply cold compresses to the painful areas to reduce inflammation.
Administer antibiotics immediately to treat the underlying infection.
Encourage the patient to perform light exercise to promote circulation.
The Correct Answer is A
Choice A Reason:
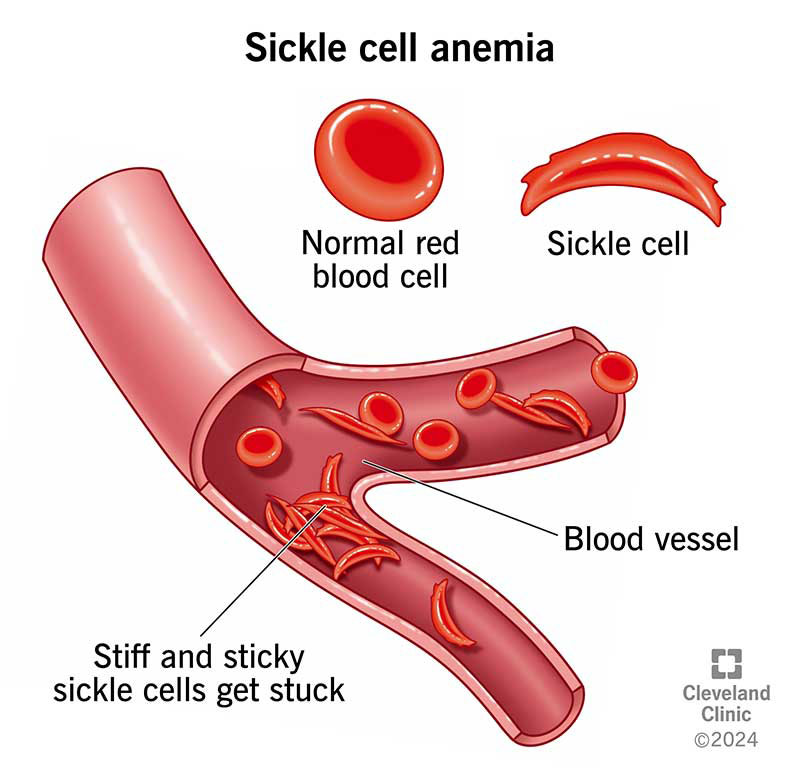
Administering intravenous fluids and pain management is the most appropriate initial intervention for a patient with sickle cell anemia presenting with severe pain, fever, and dehydration. Sickle cell crises often lead to severe pain due to vaso-occlusion, where sickled red blood cells block blood flow to various parts of the body. Intravenous fluids help to rehydrate the patient and reduce blood viscosity, which can alleviate the vaso-occlusive crisis. Pain management is crucial to provide relief and improve the patient’s comfort. This approach addresses the immediate symptoms and stabilizes the patient.
Choice B Reason:
Applying cold compresses to the painful areas is not recommended for patients with sickle cell anemia. Cold can cause vasoconstriction, which may worsen the vaso-occlusion and increase pain. Instead, warm compresses are often suggested to help dilate blood vessels and improve blood flow.
Choice C Reason:
Administering antibiotics immediately is not the primary intervention unless there is a clear indication of an infection. While fever can be a sign of infection, it can also occur due to the inflammatory response associated with a sickle cell crisis. The priority is to manage pain and dehydration first, and then evaluate the need for antibiotics based on clinical findings.
Choice D Reason:
Encouraging the patient to perform light exercise is not appropriate during an acute sickle cell crisis. Physical activity can increase oxygen demand and exacerbate the pain and vaso-occlusion. Rest and adequate hydration are more suitable to manage the crisis effectively.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
Febrile non-hemolytic transfusion reactions (FNHTRs) are common and typically present with fever, chills, and sometimes rigors. However, they do not usually cause severe symptoms such as back pain and difficulty breathing. FNHTRs are generally less severe and are caused by the recipient’s immune response to donor white blood cells or cytokines in the transfused blood.
Choice B Reason:
Allergic reactions to blood transfusions can range from mild to severe. Mild reactions may include itching, hives, and rash, while severe reactions (anaphylaxis) can cause difficulty breathing and hypotension. However, allergic reactions do not typically cause back pain, which is more indicative of a hemolytic process.
Choice C Reason:
Fluid overload, also known as transfusion-associated circulatory overload (TACO), can occur when too much blood is transfused too quickly. Symptoms include dyspnea, hypertension, and pulmonary edema. While difficulty breathing is a symptom of fluid overload, chills and back pain are not typical features.
Choice D Reason:
Acute hemolytic transfusion reaction (AHTR) is the most likely cause of the patient’s symptoms. AHTR occurs when the recipient’s immune system attacks the transfused red blood cells, leading to their destruction. This reaction can cause severe symptoms such as chills, fever, back pain, and difficulty breathing. It is a medical emergency that requires immediate intervention to prevent serious complications, including kidney failure and shock.
Correct Answer is D
Explanation
Choice A Reason:
Starting the patient on a high-calcium diet is not the most appropriate initial intervention for multiple myeloma. Multiple myeloma often leads to hypercalcemia, a condition where calcium levels in the blood are abnormally high due to bone breakdown. Increasing calcium intake can exacerbate this condition, leading to further complications such as kidney stones and impaired kidney function. Therefore, this choice is not suitable for managing the patient’s immediate symptoms.
Choice B Reason:
Encouraging the patient to increase physical activity to build bone strength is beneficial in the long term but not the most appropriate initial intervention. While weight-bearing exercises can help strengthen bones, they should be introduced gradually and under medical supervision to avoid fractures and other injuries. The immediate priority is to manage the patient’s pain and fatigue effectively.
Choice C Reason:
Advising the patient to limit fluid intake to prevent kidney damage is not appropriate. In fact, adequate hydration is crucial for patients with multiple myeloma to help flush out toxins and prevent kidney damage. Limiting fluid intake can lead to dehydration and worsen kidney function, which is already at risk due to the disease.
Choice D Reason:
Administering prescribed analgesics and educating the patient about pain management strategies is the most appropriate initial intervention. Pain management is a critical aspect of care for multiple myeloma patients, as bone pain is a common and debilitating symptom. Effective pain management improves the patient’s quality of life and allows them to participate in other therapeutic activities. Education on pain management strategies, including the use of medications, physical therapy, and complementary therapies, empowers the patient to manage their symptoms effectively.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
