A 72-year-old patient comes to the clinic complaining of sudden onset eye pain, nausea, and seeing halos around lights. The nurse notes that the patient’s pupil is mid-dilated and non-reactive to light. What is the most likely cause of these symptoms?
Optic neuritis
Macular degeneration
Narrow angle glaucoma
Cataract
The Correct Answer is C
Choice A: Optic Neuritis
Optic neuritis is an inflammation of the optic nerve that can cause pain and vision loss. The pain typically worsens with eye movement, and vision loss usually occurs in one eye. Symptoms include temporary vision loss, visual field loss, loss of color vision, and flashing lights. However, optic neuritis does not typically cause nausea or seeing halos around lights, and the pupil reaction to light is usually preserved.
Choice B: Macular Degeneration
Macular degeneration primarily affects central vision and is more common in older adults. It can cause blurred or reduced central vision, difficulty recognizing faces, and visual distortions such as straight lines appearing bent. However, it does not cause sudden onset eye pain, nausea, or seeing halos around lights. The pupil reaction to light remains normal in macular degeneration.
Choice C: Narrow Angle Glaucoma
Narrow angle glaucoma, also known as acute angle-closure glaucoma, is a medical emergency characterized by a sudden increase in intraocular pressure. Symptoms include severe eye pain, nausea, vomiting, seeing halos around lights, and a mid-dilated, non-reactive pupil. This condition occurs when the drainage angle between the iris and cornea becomes blocked, leading to a rapid rise in eye pressure. Immediate treatment is necessary to prevent permanent vision loss.
Choice D: Cataract
Cataracts cause clouding of the lens, leading to symptoms such as blurred vision, difficulty seeing at night, sensitivity to light, and seeing halos around lights. However, cataracts develop gradually and do not cause sudden onset eye pain or nausea. The pupil reaction to light is also typically normal in cataract patients.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
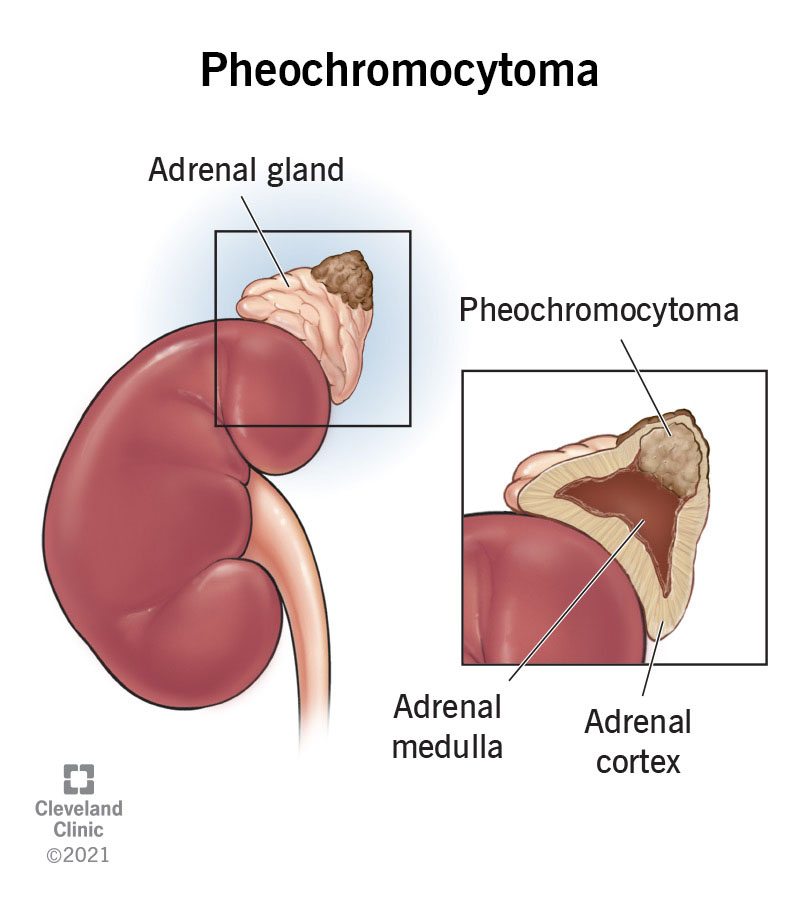
Administering an alpha-adrenergic blocker is the highest priority intervention for a patient with pheochromocytoma and severe hypertension. Pheochromocytoma causes excessive secretion of catecholamines, leading to severe hypertension. Alpha-adrenergic blockers help to control blood pressure by blocking the effects of these catecholamines, thereby reducing vasoconstriction and lowering blood pressure. This intervention is crucial to prevent hypertensive crises and associated complications such as stroke or myocardial infarction.
Choice B Reason:
Administering intravenous fluids to maintain hydration is important but not the highest priority. While maintaining hydration is essential, it does not directly address the severe hypertension caused by pheochromocytoma. Intravenous fluids can help support overall patient stability but do not specifically target the underlying cause of the hypertension.
Choice C Reason:
Monitoring blood glucose levels every 4 hours is a necessary intervention, especially since pheochromocytoma can cause hyperglycemia due to increased catecholamine levels. However, this intervention is not the highest priority compared to controlling the severe hypertension, which poses a more immediate threat to the patient’s health.
Choice D Reason:
Preparing the patient for immediate surgery to remove the tumor is a critical step in the long-term management of pheochromocytoma. However, surgery is not typically performed until the patient’s blood pressure is stabilized with medications such as alpha-adrenergic blockers. Therefore, while surgery is essential, it is not the immediate priority in the acute management of severe hypertension.
Correct Answer is A
Explanation
Choice A Reason:
Administering IV levothyroxine is the priority intervention for a patient with myxedema coma. Myxedema coma is a severe form of hypothyroidism that requires immediate thyroid hormone replacement to correct the deficiency and stabilize the patient’s condition. Intravenous levothyroxine is preferred because it provides a rapid increase in thyroid hormone levels, which is crucial for reversing the life-threatening symptoms of myxedema coma, such as hypothermia, bradycardia, and altered mental status.
Choice B Reason:
Starting broad-spectrum antibiotics is not the primary intervention for myxedema coma. While infections can precipitate myxedema coma and should be treated if present, the immediate priority is to address the severe hypothyroidism with thyroid hormone replacement. Antibiotics may be administered if an infection is suspected or confirmed, but they do not directly address the underlying thyroid hormone deficiency.
Choice C Reason:
Administering corticosteroids immediately is important but not the highest priority. Corticosteroids are often given to patients with myxedema coma to treat potential adrenal insufficiency, which can coexist with severe hypothyroidism. However, the primary intervention remains the administration of thyroid hormone replacement to correct the hypothyroid state.
Choice D Reason:
Initiating fluid restriction is not appropriate for managing myxedema coma. Patients with myxedema coma often require careful fluid management to address potential hyponatremia and maintain hemodynamic stability. Fluid restriction is not a standard intervention for this condition and does not address the critical need for thyroid hormone replacement.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
