IV potassium chloride (KCl) 60 mEq is prescribed for a 49-year-old female patient with severe hypokalemia. Which action should the nurse take?
Infuse the KCl at a maximum rate of 10 mEq/hr.
Discontinue cardiac monitoring during the infusion.
Administer the KCl as a rapid IV bolus.
Refuse to give the KCl through a peripheral venous line.
The Correct Answer is A
Choice A: Infuse the KCl at a maximum rate of 10 mEq/hr
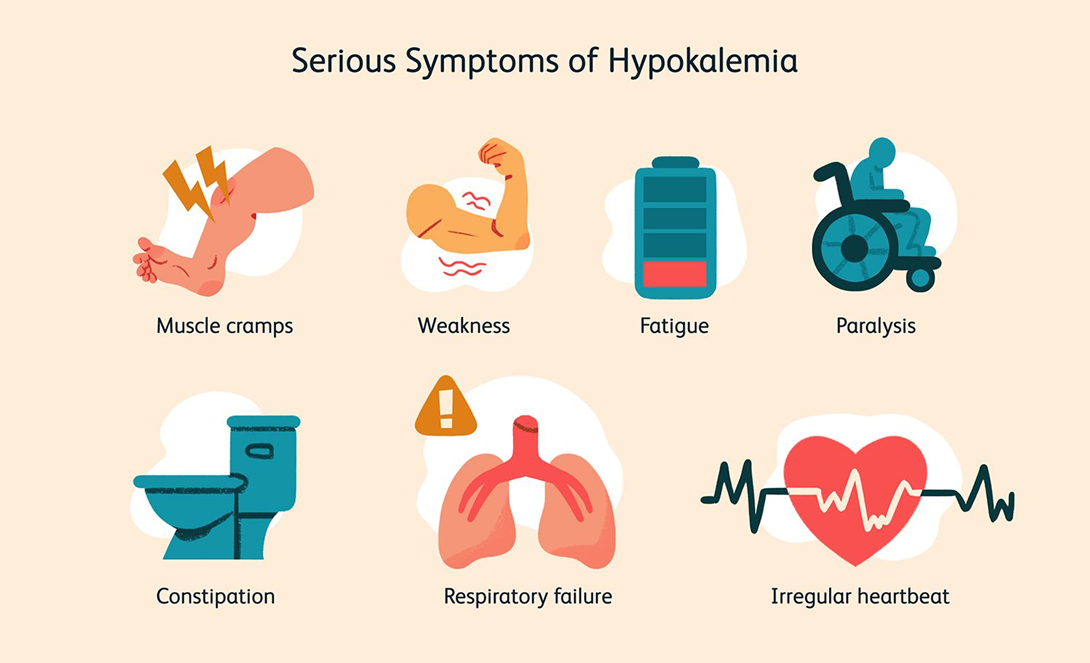
This is the correct answer. The recommended infusion rate for potassium chloride is generally not to exceed 10 mEq per hour to avoid complications such as hyperkalemia and cardiac arrhythmias. This rate ensures that the potassium is administered safely and effectively, allowing for proper monitoring and adjustment if necessary.
Choice B: Discontinue cardiac monitoring during the infusion
This choice is incorrect. Cardiac monitoring is essential during the infusion of potassium chloride, especially in patients with severe hypokalemia, due to the risk of arrhythmias and other cardiac complications. Continuous monitoring allows for the early detection of any adverse effects and timely intervention.
Choice C: Administer the KCl as a rapid IV bolus
Administering potassium chloride as a rapid IV bolus is dangerous and contraindicated. Rapid infusion can lead to severe hyperkalemia, which can cause fatal cardiac arrhythmias. Potassium chloride should always be administered slowly and diluted in an appropriate volume of fluid.
Choice D: Refuse to give the KCl through a peripheral venous line
While central lines are preferred for higher concentrations of potassium chloride due to the risk of irritation and phlebitis, peripheral lines can be used for lower concentrations and slower infusion rates. Refusing to administer potassium chloride through a peripheral line is not necessary if the infusion is properly managed and monitored.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: Promote healing by increasing the rate of the muscle remodeling process
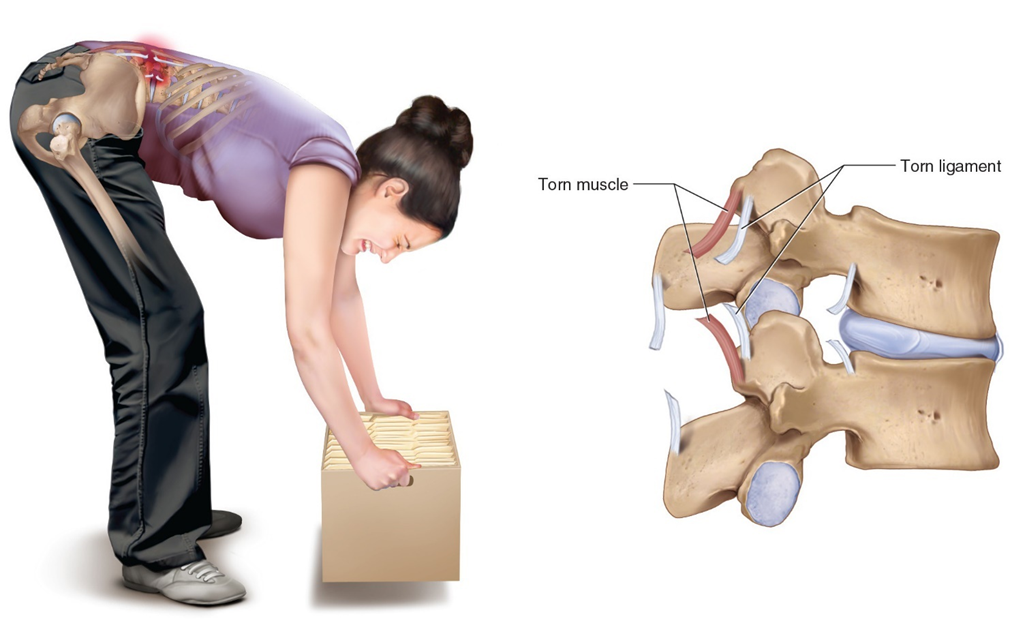
While heat can aid in the healing process by improving blood flow and nutrient delivery to the injured area, it does not specifically increase the rate of the muscle remodeling process. Muscle remodeling involves complex cellular activities that are not solely influenced by external heat application.
Choice B: Decrease pain by reducing inflammation
Heat therapy is generally not used to reduce inflammation. In fact, applying heat to an inflamed area can sometimes exacerbate the inflammation. Cold therapy is more effective for reducing inflammation, especially in the initial stages of an injury.
Choice C: Decrease pain by increasing circulation to a painful area and relaxing tense muscles
This is the correct answer. Applying heat to a painful area causes vasodilation, which increases blood flow and helps deliver oxygen and nutrients to the affected tissues. This process helps to relax tense muscles and alleviate pain. Heat therapy is particularly effective for muscle spasms, stiffness, and chronic pain conditions.
Choice D: Decrease pain by numbing pain signals
Heat therapy does not numb pain signals in the same way that cold therapy does. Cold therapy works by numbing the affected area and reducing nerve activity, which helps to alleviate pain. Heat therapy, on the other hand, works by improving circulation and relaxing muscles.
Correct Answer is ["B","C","E"]
Explanation
Choice A: Properly cleaning all reusable equipment once each day
While cleaning reusable equipment is important, it should be done after each use, not just once a day. This ensures that any potential pathogens are removed before the equipment is used on another patient, thereby preventing cross-contamination.
Choice B: Appropriately using PPE
This is a correct answer. Personal Protective Equipment (PPE) such as gloves, masks, gowns, and eye protection are essential in preventing the spread of infection. Proper use of PPE helps protect both healthcare workers and patients from exposure to infectious agents.
Choice C: Ensuring all environmental surfaces are properly cleaned, disinfected, and maintained
This is another correct answer. Regular cleaning and disinfection of environmental surfaces, such as bed rails, doorknobs, and medical equipment, are crucial in preventing the spread of infections. Maintaining a clean environment reduces the risk of healthcare-associated infections.
Choice D: Avoiding all invasive interventions
Avoiding invasive interventions is not a practical or realistic approach to preventing infections. While minimizing unnecessary invasive procedures can reduce infection risk, many invasive interventions are necessary for patient care. Instead, proper aseptic techniques should be used during these procedures to prevent infections.
Choice E: Performing hand washing or using an alcohol-based hand sanitizer before and after patient contact or procedures
This is also a correct answer. Hand hygiene is one of the most effective measures to prevent the spread of infections. Washing hands with soap and water or using an alcohol-based hand sanitizer before and after patient contact or procedures significantly reduces the transmission of pathogens.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
