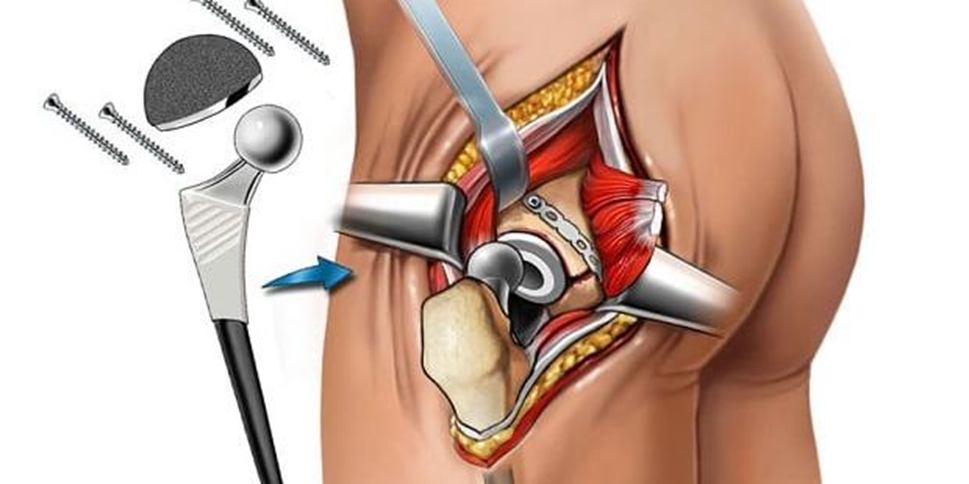
A patient who is just waking up after having hip replacement surgery is agitated and confused. Which action should the nurse take first?
Apply wrist restraints to secure IV lines.
Administer the prescribed opioid.
Take the blood pressure and pulse.
Check the oxygen (O2) saturation.
The Correct Answer is D
Choice A: Apply wrist restraints to secure IV lines
Applying wrist restraints to secure IV lines should not be the first action. Restraints are generally considered a last resort due to their potential to cause harm and distress. They should only be used when absolutely necessary and after other interventions have failed. In this scenario, the patient’s agitation and confusion could be due to hypoxia, and addressing the underlying cause is more important than immediately resorting to restraints.
Choice B: Administer the prescribed opioid
Administering the prescribed opioid is not the first action to take. While pain management is crucial, opioids can sometimes exacerbate confusion and agitation, especially in the immediate postoperative period. It is essential to first assess the patient’s vital signs and oxygen levels to rule out hypoxia or other complications before administering any medication.
Choice C: Take the blood pressure and pulse
Taking the blood pressure and pulse is important but not the immediate first action. While these vital signs provide critical information about the patient’s cardiovascular status, checking the oxygen saturation is more urgent in this context. Hypoxia can lead to agitation and confusion, and addressing it promptly can stabilize the patient more effectively.
Choice D: Check the oxygen (O2) saturation
Checking the oxygen (O2) saturation should be the first action. Hypoxia is a common cause of postoperative agitation and confusion. By assessing the patient’s oxygen levels, the nurse can quickly determine if supplemental oxygen is needed, which can help alleviate the patient’s symptoms and prevent further complications. Ensuring adequate oxygenation is a priority in the immediate postoperative period.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: True
The essential core of nursing practice indeed revolves around delivering holistic, patient-centered care. This approach integrates the art and science of nursing to ensure comprehensive care that addresses the physical, emotional, social, and spiritual needs of patients. Holistic care involves thorough assessment and evaluation to understand the patient’s overall health status and needs. Nurses provide a variety of interventions, from administering medications to performing procedures, to support patient health and recovery. Additionally, patient and caregiver teaching is crucial for empowering individuals to manage their health effectively. Nurses also play a vital role as members of the interprofessional healthcare team, collaborating with other healthcare professionals to ensure coordinated and effective care.
Choice B: False
The statement that the essential core of nursing practice is not to deliver holistic, patient-centered care is incorrect. Holistic, patient-centered care is a fundamental principle of nursing practice. It emphasizes the importance of treating the whole person rather than just the symptoms of a disease. This approach ensures that care is tailored to the individual needs of each patient, promoting better health outcomes and patient satisfaction. By focusing on holistic care, nurses can address the diverse aspects of a patient’s well-being, including their physical, emotional, social, and spiritual needs.
Correct Answer is A
Explanation
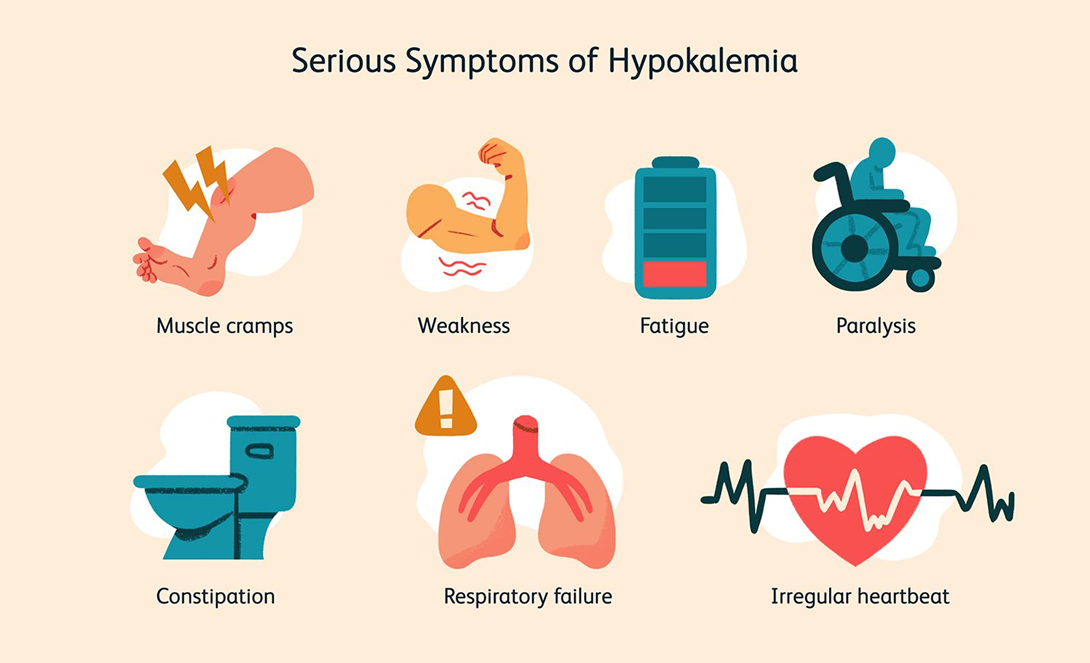
Choice A: Infuse the KCl at a maximum rate of 10 mEq/hr
This is the correct answer. The recommended infusion rate for potassium chloride is generally not to exceed 10 mEq per hour to avoid complications such as hyperkalemia and cardiac arrhythmias. This rate ensures that the potassium is administered safely and effectively, allowing for proper monitoring and adjustment if necessary.
Choice B: Discontinue cardiac monitoring during the infusion
This choice is incorrect. Cardiac monitoring is essential during the infusion of potassium chloride, especially in patients with severe hypokalemia, due to the risk of arrhythmias and other cardiac complications. Continuous monitoring allows for the early detection of any adverse effects and timely intervention.
Choice C: Administer the KCl as a rapid IV bolus
Administering potassium chloride as a rapid IV bolus is dangerous and contraindicated. Rapid infusion can lead to severe hyperkalemia, which can cause fatal cardiac arrhythmias. Potassium chloride should always be administered slowly and diluted in an appropriate volume of fluid.
Choice D: Refuse to give the KCl through a peripheral venous line
While central lines are preferred for higher concentrations of potassium chloride due to the risk of irritation and phlebitis, peripheral lines can be used for lower concentrations and slower infusion rates. Refusing to administer potassium chloride through a peripheral line is not necessary if the infusion is properly managed and monitored.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
