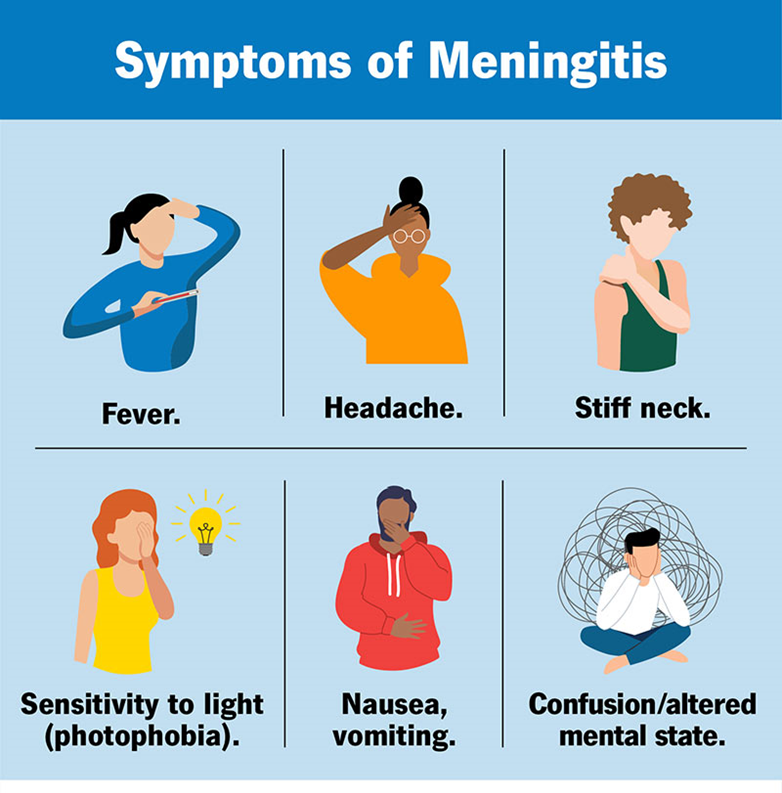
A client is admitted with bacterial meningitis. Which nursing intervention is the highest priority for this client?
Strict monitoring of hourly intake and output
Managing pain through drug and non-drug methods
Assessing neurological status at least every 2 to 4 hours
Decreasing environmental stimuli
The Correct Answer is C
Choice A reason:
Strict monitoring of hourly intake and output is important for managing fluid balance and detecting potential complications such as dehydration or fluid overload1. However, it is not the highest priority in the acute phase of bacterial meningitis. The primary concern is to monitor for signs of increased intracranial pressure (ICP) and neurological deterioration.
Choice B reason:
Managing pain through drug and non-drug methods is essential for patient comfort and overall well-being. Pain management can help reduce stress and improve the patient’s ability to rest and recover. However, it is not the highest priority compared to monitoring neurological status, which can provide early indications of complications such as increased ICP or seizures.
Choice C reason:
Assessing neurological status at least every 2 to 4 hours is the highest priority for a client with bacterial meningitis. This frequent assessment helps detect early signs of neurological deterioration, increased ICP, and other complications. Early detection and intervention are crucial in preventing severe outcomes and improving the patient’s prognosis.
Choice D reason:
Decreasing environmental stimuli is important to reduce stress and prevent exacerbation of symptoms such as headache and photophobia. While this intervention is beneficial, it is not as critical as frequent neurological assessments in the acute management of bacterial meningitis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason:
Hypotension (low blood pressure), tachycardia (rapid heart rate), and lethargy are critical symptoms that can indicate a life-threatening condition such as shock or severe dehydration. Hypotension can lead to inadequate perfusion of vital organs, resulting in multi-organ failure if not promptly addressed1. Tachycardia is often a compensatory mechanism for hypotension, and lethargy indicates decreased cerebral perfusion. Immediate intervention is required to stabilize the patient’s condition and prevent further deterioration.
Choice B reason:
Dizziness with a headache rated 7/10 on the numeric scale is concerning but not immediately life-threatening. These symptoms could indicate a variety of conditions, such as migraine, vertigo, or even a mild concussion. While the patient should be assessed and treated, they do not present the same immediate risk as hypotension and tachycardia.
Choice C reason:
Abdominal pain, hypertension (high blood pressure), and constipation are symptoms that need medical attention but are not immediately life-threatening. Hypertension can lead to serious complications if left untreated, but it does not require the same urgent intervention as hypotension. Abdominal pain and constipation, while uncomfortable and potentially indicative of underlying issues, do not pose an immediate threat to life.
Choice D reason:
Febrile (fever), tachycardia, and vomiting are symptoms that suggest an infection or other acute illness. While these symptoms are concerning and need prompt evaluation, they do not pose the same immediate risk as hypotension and tachycardia. Fever and vomiting can lead to dehydration, but this typically develops over a longer period compared to the rapid deterioration seen with hypotension.
Correct Answer is B
Explanation
Choice A Reason:
Decrease protein intake: This is not typically recommended for clients with Cushing’s disease. Protein is essential for maintaining muscle mass and overall health. Clients with Cushing’s disease often experience muscle weakness and wasting, so adequate protein intake is crucial to help counteract these effects. Therefore, decreasing protein intake would not be beneficial.
Choice B Reason:
Restrict sodium intake: Clients with Cushing’s disease often suffer from hypertension (high blood pressure) due to the excess cortisol in their bodies. High sodium intake can exacerbate this condition by increasing blood pressure even further. Therefore, it is crucial to restrict sodium intake to help manage hypertension and reduce the risk of cardiovascular complications. Foods high in sodium include processed foods, canned soups, and salty snacks. The recommended daily sodium intake for most adults is less than 2,300 milligrams, but for those with hypertension, it is often advised to consume even less.
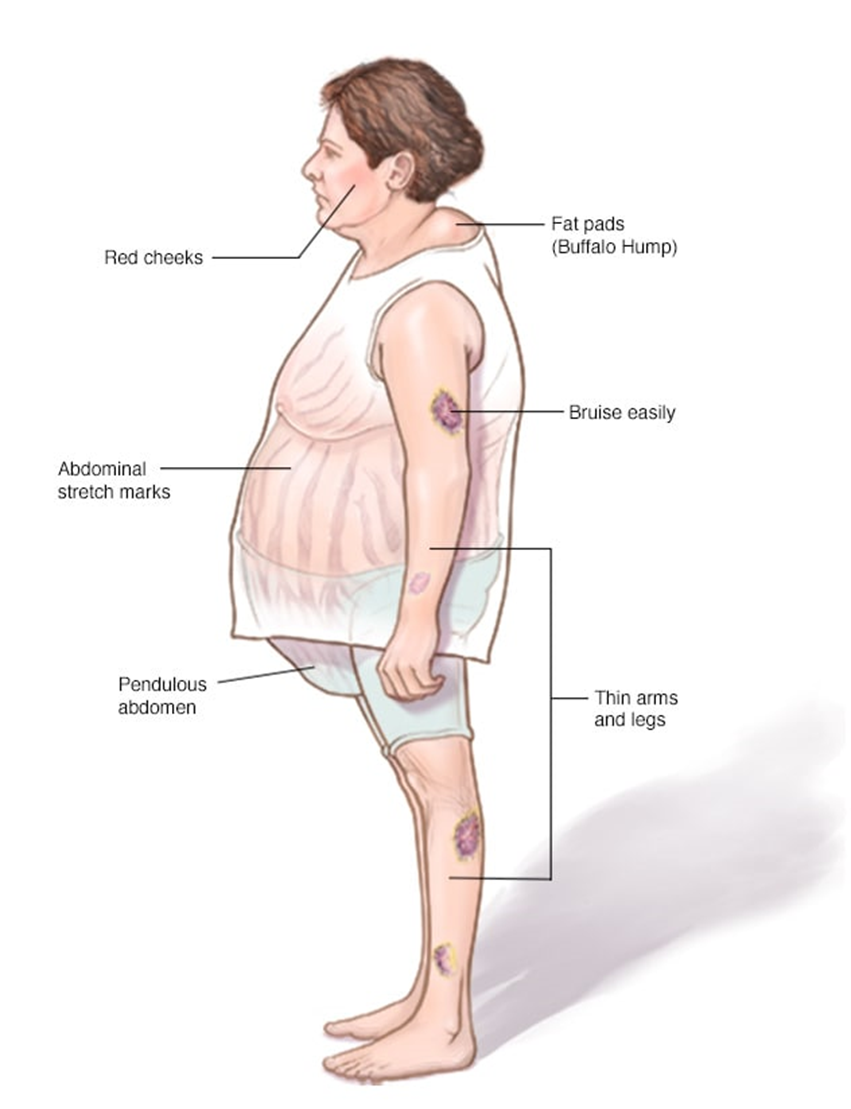
Choice C Reason:
Limit intake of potassium-rich foods: This is not a standard recommendation for clients with Cushing’s disease. In fact, potassium is often beneficial as it can help counteract the effects of sodium and lower blood pressure. Potassium-rich foods include bananas, oranges, spinach, and sweet potatoes. Limiting these foods would not be advantageous and could potentially worsen hypertension.
Choice D Reason:
Increase carbohydrate intake: Increasing carbohydrate intake is not typically recommended for clients with Cushing’s disease. Excess cortisol can lead to increased blood sugar levels and a higher risk of developing diabetes. Therefore, it is important to manage carbohydrate intake carefully to avoid spikes in blood sugar. Instead, a balanced diet with a focus on complex carbohydrates, lean proteins, and healthy fats is recommended.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
