A client who had a bronchoscopy 2 hours ago asks for a drink of water. What action would the nurse take initially to assure client safety?
Assess the client’s gag reflex before giving any food or water.
Provide the client with ice chips instead of a drink of water.
Contact the primary healthcare provider and get the appropriate orders.
Let the client have a small sip to evaluate the ability to swallow.
The Correct Answer is A
Choice A Reason:
Assessing the client’s gag reflex before giving any food or water is crucial after a bronchoscopy. The procedure involves the use of local anesthesia to numb the throat, which can impair the gag reflex and increase the risk of aspiration. Ensuring that the gag reflex has returned before allowing the client to eat or drink helps prevent choking and aspiration, which are serious complications.
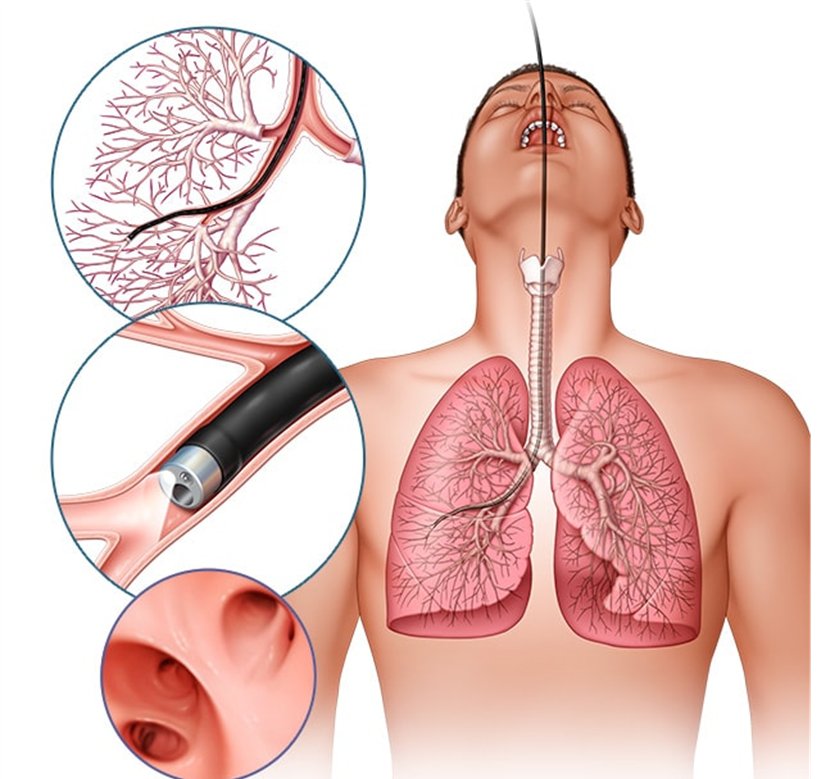
Choice B Reason:
Providing the client with ice chips instead of a drink of water is not the best initial action. While ice chips may seem like a safer option, they still pose a risk of aspiration if the gag reflex has not fully returned. The priority is to first assess the gag reflex to ensure the client can safely swallow.
Choice C Reason:
Contacting the primary healthcare provider and getting the appropriate orders is not necessary as the first action. The nurse can independently assess the gag reflex, which is a standard nursing practice after procedures involving throat anesthesia. If there are concerns after the assessment, then contacting the healthcare provider would be appropriate.
Choice D Reason:
Letting the client have a small sip to evaluate the ability to swallow is not safe without first assessing the gag reflex. This approach could lead to aspiration if the gag reflex has not returned. The initial step should always be to assess the gag reflex to ensure the client can safely swallow liquids.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["C","E"]
Explanation
Choice A: Formed stool in collection pouch
Formed stool in the collection pouch is not expected in an ileostomy. The output from an ileostomy is typically liquid to semi-liquid because the ileum does not absorb as much water as the colon. If formed stool is present, it may indicate a blockage or other issue that needs to be addressed.
Choice B: Stoma is edematous and bleeding
An edematous and bleeding stoma is not a normal finding and may indicate complications such as infection, trauma, or poor stoma care. The stoma should be moist and pink, but not swollen or bleeding. Persistent bleeding or significant edema should be reported to a healthcare provider immediately.
Choice C: Stoma is pink and shiny
A pink and shiny stoma is a sign that the ileostomy is functioning well. This indicates good blood flow and healthy tissue. The stoma should always appear moist and pink, similar to the inside of the mouth. Any deviation from this appearance, such as a pale, dark, or dry stoma, should be evaluated by a healthcare professional.
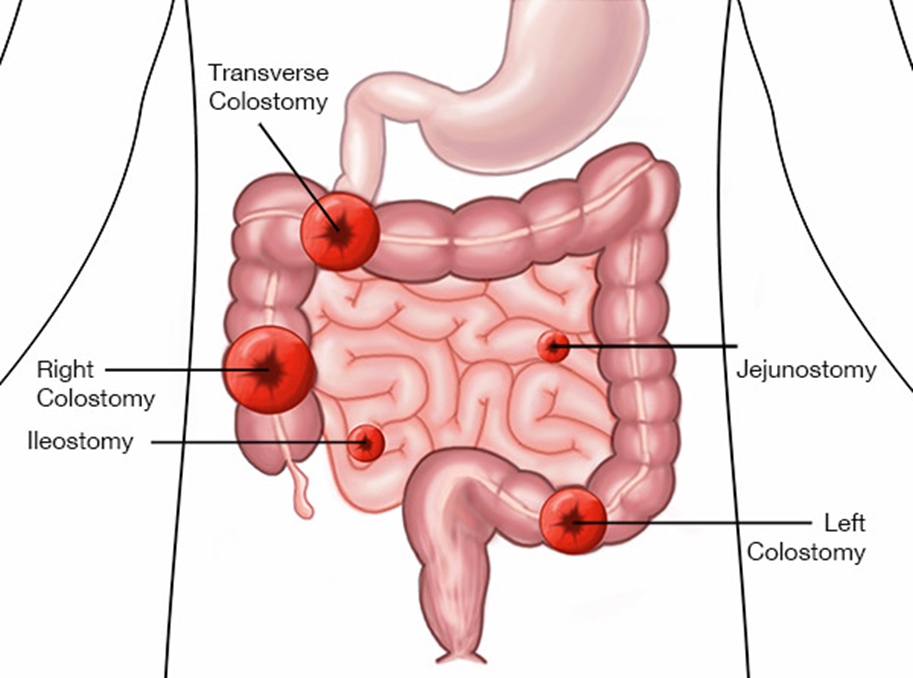
Choice D: Skin excoriation around the stoma
Skin excoriation around the stoma is not a normal finding and suggests that the skin is being irritated by the stoma output or the ostomy appliance. Proper skin care and fitting of the ostomy appliance are essential to prevent skin breakdown. If excoriation occurs, it should be treated promptly to prevent further complications.
Choice E: Mucus liquid flows from the stoma
Mucus liquid flowing from the stoma is expected in an ileostomy. The output is typically liquid to semi-liquid and may contain mucus, which is normal for the small intestine. This type of output indicates that the ileostomy is functioning as intended.
Correct Answer is D
Explanation
Choice A reason: No change to the heparin rate is not appropriate in this scenario. The normal range for PTT is generally between 25 to 35 seconds. However, for a client on heparin therapy, the target PTT is typically 1.5 to 2.5 times the normal range, which would be approximately 60 to 80 seconds. Since the client’s PTT is only 25 seconds, it indicates that the blood is clotting too quickly, and the heparin dose is insufficient.
Choice B reason: Decreasing the heparin rate would further reduce the anticoagulant effect, which is not advisable given the current PTT of 25 seconds. Lowering the heparin rate could increase the risk of thrombus formation and worsen the deep vein thrombosis (DVT) condition.
Choice C reason: Stopping heparin and starting warfarin is not an immediate solution. Warfarin takes several days to achieve its full anticoagulant effect, and during this transition period, the client would be at risk of clot formation. Heparin provides immediate anticoagulation, which is crucial in the acute management of DVT.
Choice D reason: Increasing the heparin rate is the correct action. The current PTT of 25 seconds is below the therapeutic range for a client on heparin therapy. Increasing the heparin rate will help achieve the desired anticoagulant effect, prolonging the PTT to the target range of 60 to 80 seconds.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
