Patient Data
The nurse is planning care for the client
Complete the diagram by dragging from the choices area to specify which condition the client is most likely experiencing, two actions the nurse should take to address that condition, and two parameters the nurse should monitor to assess the client's progress.
The Correct Answer is []
The nurse should:
- Raise the head of the bed to aid in breathing.
- Change to a face mask for oxygen delivery to address hypoxia.
The nurse should monitor:
- Lung sounds to assess the progression of pneumonia.
- Oxygen saturation to ensure the patient is receiving adequate oxygen.
Choice A reason: Increasing IV fluids is important in the care of pneumonia patients to prevent dehydration, especially if the patient has fever and increased respiratory rate which can lead to fluid loss. However, in this case, the patient’s blood pressure is stable, and there is no indication of dehydration, so this would not be the immediate action.
Choice B reason: Raising the head of the bed can help improve the patient’s breathing by reducing pressure on the chest and aiding in lung expansion. This is a standard care practice for patients with respiratory difficulties and is particularly beneficial for those with pneumonia to facilitate easier breathing.
Choice C reason: Bronchodilator nebulization can help open airways and improve breathing in patients with respiratory conditions. While it may be used in the treatment of pneumonia, it is not the primary intervention for hypoxia.
Choice D reason: Changing to a face mask for oxygen delivery is a critical intervention for a patient experiencing hypoxia. The patient’s oxygen saturation is 88% on 2 L/minute via nasal cannula, which is below the normal range of 95-100%3. A face mask can deliver higher concentrations of oxygen, which is necessary to address the patient’s hypoxia.
Choice E reason: Calling a rapid response team is necessary if the patient’s condition is deteriorating rapidly and requires immediate medical intervention. In this scenario, while the patient is hypoxic, there is no indication of acute decompensation that would necessitate a rapid response team at this moment.
Choice F reason: Pneumothorax, or collapsed lung, would present with sudden chest pain and shortness of breath. The patient’s history and symptoms are more consistent with pneumonia rather than pneumothorax.
Choice G reason: Hypoventilation refers to decreased breathing efficiency, leading to increased levels of carbon dioxide in the blood. While the patient does have difficulty breathing, the primary issue seems to be the impaired oxygen exchange due to pneumonia, rather than hypoventilation.
Choice H reason: Atelectasis is the collapse of part of the lung, which can occur after surgery or with bedridden patients. This patient’s symptoms are more indicative of an infectious process rather than atelectasis.
Choice I reason: Hypoxia is a condition where the body or a region of the body is deprived of adequate oxygen supply. Given the patient’s low oxygen saturation level and bilateral lower lobe pneumonia, hypoxia is the most likely condition the patient is experiencing.
Choice J reason: Monitoring lung sounds is essential for assessing the effectiveness of treatment and progression of pneumonia. Diminished lung sounds can indicate poor air movement due to the infection.
Choice K reason: Changes in the level of consciousness can indicate worsening hypoxia and should be monitored closely. A decrease in consciousness can be a sign of inadequate brain oxygenation.
Choice L reason: Oxygen saturation is a direct measure of the patient’s respiratory status and should be monitored to assess the effectiveness of oxygen therapy and overall progression.
Choice M reason: While heart rhythm should be monitored in all patients, it is not the most specific parameter for assessing the progression of pneumonia or hypoxia.
Choice N reason: Temperature should be monitored to assess for fever, which can indicate infection or inflammation. However, it is not as directly related to respiratory function as oxygen saturation and lung sounds are in the context of pneumonia.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","D","E"]
Explanation
Choice A reason: Obtaining a history of allergic reactions is crucial because the child will be exposed to various substances during cardiac catheterization, such as contrast dye, which could potentially cause an allergic reaction.
Choice B reason: Documenting lying, sitting, and standing blood pressures is important to assess for orthostatic hypotension, which could indicate volume depletion or cardiovascular problems that need to be addressed before the procedure.
Choice C reason: Performing a mini mental exam on the child is not typically part of the pre-procedure assessment for cardiac catheterization, especially given the young age of the child.
Choice D reason: Determining when the child last ate is essential because the child needs to have an empty stomach to reduce the risk of aspiration during sedation.
Choice E reason: Locating and marking the pedal pulses is important to establish baseline data so that post-procedure, any changes in the strength or presence of these pulses can be quickly identified, indicating potential complications.
Choice F reason: Measuring the child’s height and weight is generally part of a routine assessment but is not specifically focused on the pre-cardiac catheterization assessment unless dosing of medication or anesthesia is required based on weight.
Correct Answer is C
Explanation
Choice A reason: Offering supplemental formula feedings is not the first-line action for inverted nipples as it does not address the issue and may lead to nipple confusion, potentially complicating future breastfeeding attempts.
Choice B reason: Teaching about the use of a breast pump is beneficial for milk expression but does not directly assist with the immediate concern of latching issues due to inverted nipples.
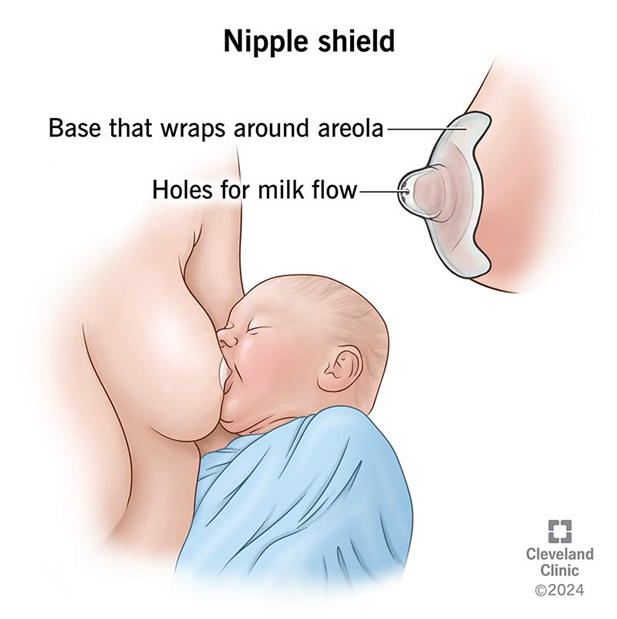
Choice C reason: Using a breast shield can be helpful for mothers with inverted nipples. It can temporarily draw out the nipple, allowing the baby to latch on more easily. This tool acts as a bridge between the breast and the baby's mouth, facilitating breastfeeding while the mother works on long-term solutions for her inverted nipples.
Choice D reason: Encouraging the use of ice on the areola may temporarily stiffen the nipple, but it is not a recommended practice for addressing inverted nipples as it can cause discomfort and may not be effective in promoting a successful latch.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
