Surgical repair for patent ductus arteriosus (PDA) is done to prevent the complication of
Increased pulmonary vascular congestion
decreased workload on the jet side of the heart
pulmonary Infection
Right-to-left shunt of blood
The Correct Answer is A
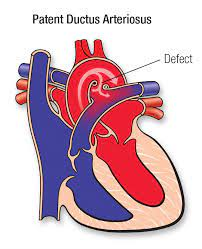
PDA is a congenital heart defect where a blood vessel called the ductus arteriosus, which is supposed to close shortly after birth, remains open. This allows oxygenated blood from the aorta to flow back into the pulmonary artery, leading to increased pulmonary blood flow and congestion. Over time, this can lead to increased pulmonary vascular congestion and potentially cause complications such as pulmonary hypertension and heart failure.
Surgical repair of PDA, often through a procedure known as ligation or closure of the ductus arteriosus, is performed to stop this abnormal blood flow and prevent the associated complications, particularly the increase in pulmonary vascular congestion.
The other options (B, C, and D) are not the primary complications associated with PDA and surgical repair is not performed primarily to address these issues:
B. Decreased workload on the left side of the heart is not a primary reason for surgical repair of PDA, although it can be a potential benefit of closing the ductus arteriosus.
C. Pulmonary infection is not a direct complication of PDA, but the increased pulmonary blood flow associated with a large PDA can make the lungs more susceptible to respiratory infections.
D. Right-to-left shunt of blood is not a typical complication of PDA. PDA typically involves left-to-right shunting of blood, with oxygenated blood flowing back into the pulmonary circulation, leading to complications related to increased pulmonary blood flow.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Cardioversion involves delivering an electrical shock to the heart to restore a normal rhythm. While it may be used for certain types of tachyarrhythmias in adults, it is typically not the first-line treatment for SVT in pediatric patients.
In pediatric patients with SVT, the initial management options often include:
B. Vagal maneuvers: Non-invasive maneuvers like the Valsalva maneuver or carotid sinus massage can be attempted to try and break the SVT rhythm.
C. Adenosine: Adenosine is often the first-line medication used for terminating SVT in pediatric patients. It is given intravenously in a controlled setting under medical supervision.
D. Continue to monitor for 30 minutes: After successful termination of SVT, it's important to continue monitoring the child's heart rhythm and vital signs to ensure that the arrhythmia does not recur.
In pediatric patients, the decision to use cardioversion is usually reserved for situations where other methods, including medications and vagal maneuvers, have not been successful or if the child is unstable. Cardioversion in pediatric patients is performed under sedation or anesthesia to minimize discomfort.
Therefore, while cardioversion may be used in some cases, it is not the initial or most common approach for treating SVT in pediatric patients, making option A the answer to the question.
Correct Answer is A
Explanation
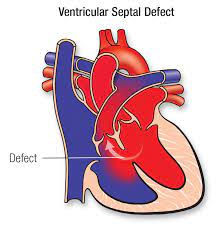
Infants with congenital heart defects, including VSD, may have increased caloric needs due to the added work of their hearts. Congestive heart failure can lead to poor weight gain and failure to thrive. Therefore, increasing the caloric density of the formula is a common approach to providing the necessary nutrition for growth and development. This can be achieved by using specialized high-calorie infant formulas or fortifying breast milk.
The other options are not the primary supportive measures for an infant with congestive heart failure in this context:
B. Oxygen therapy to ensure oxygen saturation is > 98%: While oxygen therapy may be necessary for infants with congenital heart defects, it is not the primary supportive measure to address failure to thrive. Oxygen therapy primarily aims to ensure adequate oxygenation but does not directly address caloric intake.
C. Sedatives to keep the infant from crying: The use of sedatives is not a typical approach to managing congestive heart failure in infants. Addressing the underlying cause, optimizing nutrition, and providing supportive care are more appropriate strategies.
D. Emergent surgical correction of the defect: Surgical correction of a VSD is typically considered for specific indications, such as significant hemodynamic compromise, but it is not the first-line intervention for all cases of VSD, especially if the primary concern is failure to thrive. Treatment decisions for VSD are made based on the specific clinical presentation and severity of the defect.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
