The next 3 questions relate to this case study:
Select 4 appropriate interventions for the prevention and management of chemotherapy-induced nausea and vomiting (CINV) in Ms. Anderson.
Offer peppermint aromatherapy during and after chemotherapy.
Administer antiemetics before chemotherapy.
Keep Ms. Anderson NPO for the duration of the chemotherapy.
Encourage the patient to eat and drink when not nauseated.
Offer small sips of ginger ale.
Encourage Ms. Anderson to eat a high-protein meal prior to the chemotherapy infusion.
Correct Answer : A,B,D,E
Choice A reason:
Offering peppermint aromatherapy during and after chemotherapy can be an effective non-pharmacological intervention for managing chemotherapy-induced nausea and vomiting (CINV). Aromatherapy with peppermint oil has been shown to reduce nausea and improve comfort in patients undergoing chemotherapy. The scent of peppermint can have a calming effect on the gastrointestinal system, helping to alleviate nausea. This intervention is easy to implement and can be used alongside other treatments to enhance patient comfort.
Choice B reason:
Administering antiemetics before chemotherapy is a standard practice for preventing CINV. Antiemetics, such as 5-HT3 receptor antagonists (e.g., ondansetron), NK1 receptor antagonists (e.g., aprepitant), and corticosteroids (e.g., dexamethasone), are commonly used to prevent nausea and vomiting associated with chemotherapy. These medications are most effective when given prophylactically, before the onset of symptoms. Administering antiemetics before chemotherapy helps to block the pathways that trigger nausea and vomiting, providing better control over these symptoms.
Choice C reason:
Keeping Ms. Anderson NPO (nothing by mouth) for the duration of the chemotherapy is not recommended for managing CINV. Keeping patients NPO can lead to dehydration and malnutrition, which can worsen their overall condition. Instead, patients should be encouraged to eat small, frequent meals and stay hydrated to maintain their strength and well-being. Proper nutrition and hydration are essential for supporting the body’s ability to tolerate chemotherapy and recover from its side effects.
Choice D reason:
Encouraging the patient to eat and drink when not nauseated is an important strategy for managing CINV. Eating small, frequent meals and staying hydrated can help maintain energy levels and prevent dehydration. Patients should be advised to eat bland, easy-to-digest foods and avoid foods that are greasy, spicy, or have strong odors, as these can exacerbate nausea. Encouraging patients to eat and drink when they feel well can help them maintain their nutritional status and improve their overall tolerance to chemotherapy.
Choice E reason:
Offering small sips of ginger ale can help manage nausea. Ginger has natural antiemetic properties and can be effective in reducing nausea and vomiting. Ginger ale, ginger tea, or ginger candies can be soothing and help settle the stomach. This simple intervention can be easily incorporated into the patient’s routine and can provide relief from mild to moderate nausea.
Choice F reason:
Encouraging Ms. Anderson to eat a high-protein meal prior to the chemotherapy infusion is not typically recommended for managing CINV. High-protein meals can be harder to digest and may increase the risk of nausea. Instead, patients should be advised to eat light, bland meals before chemotherapy to minimize the risk of nausea and vomiting. Light meals are easier on the stomach and less likely to trigger gastrointestinal discomfort.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: Alkalosis
Alkalosis occurs when the blood pH is higher than the normal range, specifically above 7.45. This condition indicates that the blood is too alkaline. Causes of alkalosis can include hyperventilation, loss of stomach acid through vomiting, or an overuse of diuretics. Since a blood pH of 7.21 is below the normal range, it does not indicate alkalosis.
Choice B: Normal Blood pH
The normal pH range for blood is between 7.35 and 7.45. This range is crucial for the body’s metabolic processes and enzyme functions. A blood pH of 7.21 is below this range, indicating an abnormal condition.
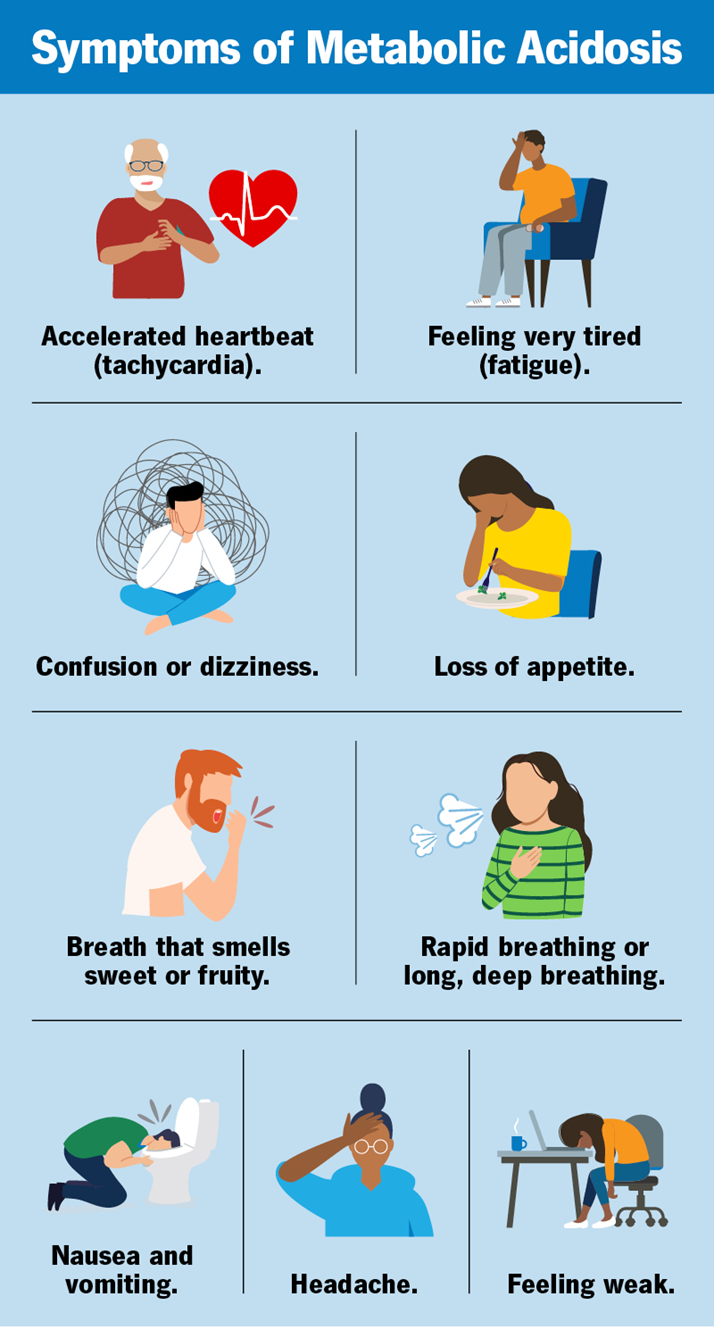
Choice C: Acidosis
Acidosis is the correct answer. It occurs when the blood pH drops below 7.35, indicating that the blood is too acidic. A pH of 7.21 is significantly below the normal range, confirming acidosis. This condition can result from various factors, including respiratory issues that lead to an accumulation of carbon dioxide or metabolic problems that increase acid production or decrease bicarbonate levels.
Choice D: Hyperkalemia
Hyperkalemia refers to an elevated level of potassium in the blood, not a change in blood pH. While hyperkalemia can be associated with acidosis, it is not defined by the pH level itself. Therefore, a blood pH of 7.21 does not directly indicate hyperkalemia.
Correct Answer is ["A","C","E"]
Explanation
Choice A: Monitor for signs and symptoms of infection
Monitoring for signs and symptoms of infection is a fundamental strategy in infection prevention. Early detection of infections allows for timely intervention, which can prevent the spread of pathogens and reduce the severity of the infection. Common signs and symptoms include fever, redness, swelling, pain, and discharge. Regular monitoring helps healthcare providers identify infections early and take appropriate actions, such as isolating the patient or starting treatment.
Choice B: Provide all patients with bottled water
Providing all patients with bottled water is not a standard infection prevention strategy. While ensuring access to clean drinking water is important, it is not specifically aimed at preventing infections. In healthcare settings, tap water is usually safe to drink if it meets regulatory standards. Bottled water may be provided in certain situations, such as during an outbreak of waterborne pathogens, but it is not a routine infection prevention measure.
Choice C: Provide education on infection prevention
Providing education on infection prevention is crucial for both healthcare providers and patients. Education helps individuals understand how infections spread and what measures they can take to prevent them. This includes proper hand hygiene, respiratory etiquette, and the importance of vaccinations. Educating patients and staff can significantly reduce the incidence of healthcare-associated infections by promoting adherence to infection control practices.
Choice D: Request an antibiotic order for a febrile patient
Requesting an antibiotic order for a febrile patient is not an infection prevention strategy but rather a treatment approach. Antibiotics are used to treat bacterial infections, not to prevent them. Overuse of antibiotics can lead to antibiotic resistance, making it crucial to use them judiciously and only when necessary. Infection prevention focuses on measures to prevent the occurrence of infections rather than treating them once they occur.
Choice E: Create a clean, safe environment
Creating a clean, safe environment is essential for infection prevention in healthcare settings. This involves regular cleaning and disinfection of surfaces, proper waste disposal, and maintaining hygiene standards. A clean environment reduces the risk of healthcare-associated infections by minimizing the presence of pathogens. Effective cleaning protocols and environmental controls are critical components of infection prevention strategies.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
