The following 4 questions pertain to this case study:
Indicate which nursing interventions the post-surgical unit nurse should complete. (Select all that apply)
Changing the patient’s position every 3 to 4 hours.
Provide adequate and regular pain medication.
Encourage deep breathing and coughing.
Place the conscious patient in a supine position with the head of the bed elevated.
Encourage bed rest for the first 4 hours after surgery.
Correct Answer : A,B,C,D
Choice A reason:
Changing the patient’s position every 3 to 4 hours is crucial to prevent complications such as pressure ulcers and deep vein thrombosis (DVT). Immobility can lead to the development of pressure ulcers, especially in patients who are bedridden or have limited mobility. Regular repositioning helps to alleviate pressure on vulnerable areas of the body, promoting better circulation and preventing skin breakdown. Additionally, changing positions can help in preventing DVT by encouraging blood flow and reducing the risk of blood clots forming in the legs.
Choice B reason:
Providing adequate and regular pain medication is essential for postoperative care to ensure patient comfort and facilitate recovery. Pain management is a critical aspect of postoperative care as unmanaged pain can lead to complications such as increased heart rate, hypertension, and delayed wound healing. Adequate pain control allows the patient to participate in necessary activities such as deep breathing exercises and ambulation, which are vital for preventing complications like pneumonia and promoting overall recovery. Pain medication should be administered as prescribed, and the patient’s pain levels should be regularly assessed and documented.
Choice C reason:
Encouraging deep breathing and coughing is vital for preventing respiratory complications such as atelectasis and pneumonia. After surgery, patients are at risk of developing these complications due to the effects of anesthesia and prolonged immobility. Deep breathing exercises help to expand the lungs fully, improving oxygenation and preventing the collapse of alveoli. Coughing helps to clear secretions from the airways, reducing the risk of infection. Nurses should instruct patients on how to perform these exercises effectively and encourage them to do so regularly.
Choice D reason:
Placing the conscious patient in a supine position with the head of the bed elevated is important for maintaining airway patency and promoting optimal respiratory function. Elevating the head of the bed helps to reduce the risk of aspiration and improves lung expansion, facilitating better breathing. This position is particularly beneficial for patients who may have residual effects of anesthesia or are at risk of respiratory complications. It also helps in reducing the workload on the heart and improving overall comfort.
Choice E reason:
Encouraging bed rest for the first 4 hours after surgery is generally not recommended as early mobilization is crucial for preventing complications such as DVT, pulmonary embolism, and muscle atrophy. While it is important to ensure that the patient is stable before encouraging movement, prolonged bed rest can lead to adverse outcomes. Instead, patients should be encouraged to engage in light activities as soon as they are able, under the supervision of healthcare professionals. This helps to promote circulation, improve respiratory function, and enhance overall recovery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: Alkalosis
Alkalosis occurs when the blood pH is higher than the normal range, specifically above 7.45. This condition indicates that the blood is too alkaline. Causes of alkalosis can include hyperventilation, loss of stomach acid through vomiting, or an overuse of diuretics. Since a blood pH of 7.21 is below the normal range, it does not indicate alkalosis.
Choice B: Normal Blood pH
The normal pH range for blood is between 7.35 and 7.45. This range is crucial for the body’s metabolic processes and enzyme functions. A blood pH of 7.21 is below this range, indicating an abnormal condition.
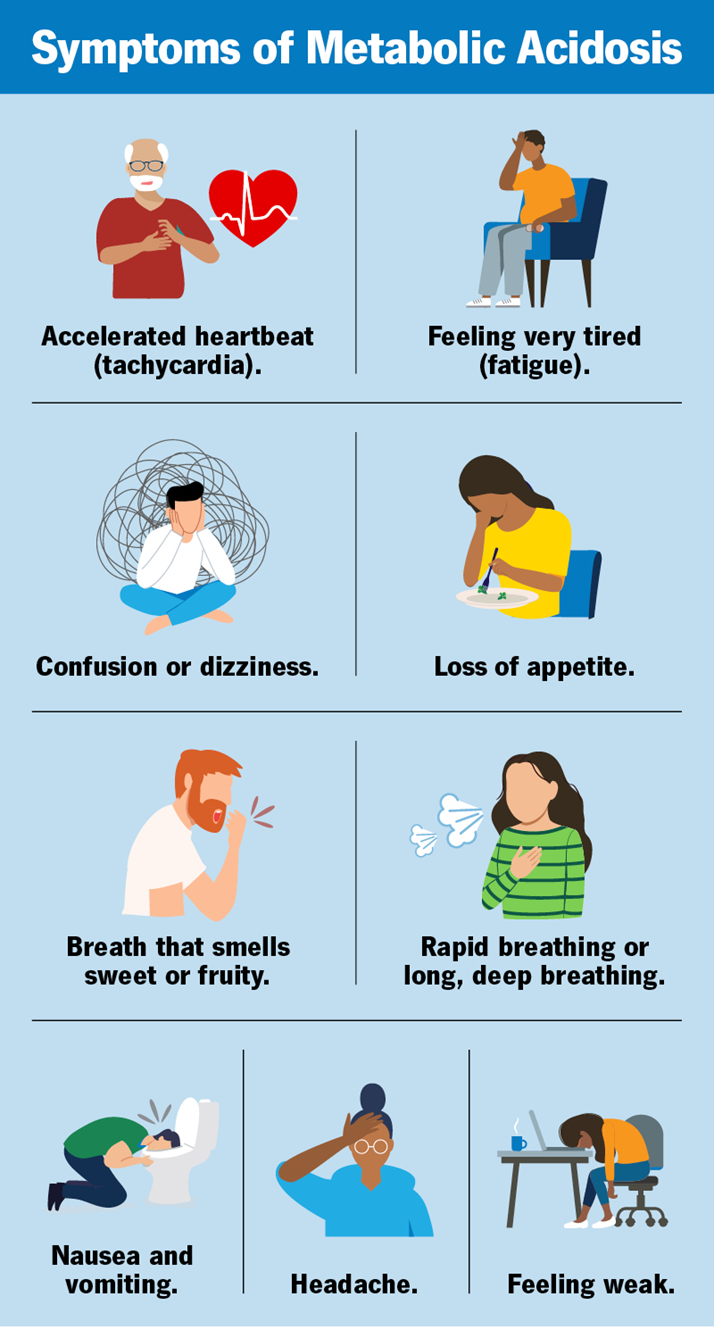
Choice C: Acidosis
Acidosis is the correct answer. It occurs when the blood pH drops below 7.35, indicating that the blood is too acidic. A pH of 7.21 is significantly below the normal range, confirming acidosis. This condition can result from various factors, including respiratory issues that lead to an accumulation of carbon dioxide or metabolic problems that increase acid production or decrease bicarbonate levels.
Choice D: Hyperkalemia
Hyperkalemia refers to an elevated level of potassium in the blood, not a change in blood pH. While hyperkalemia can be associated with acidosis, it is not defined by the pH level itself. Therefore, a blood pH of 7.21 does not directly indicate hyperkalemia.
Correct Answer is ["A","B","C","D","E"]
Explanation
Choice A: Collect patient information
The first step in the nursing process is to collect patient information, also known as the assessment phase. During this phase, the nurse gathers comprehensive data about the patient’s health status, including medical history, physical examination findings, and any relevant diagnostic test results. This information forms the foundation for identifying the patient’s needs and planning appropriate care.
Choice B: Identify any clinical problems
After collecting patient information, the next step is to identify any clinical problems, also known as the diagnosis phase. In this phase, the nurse analyzes the assessment data to determine the patient’s health issues or potential risks. This step involves critical thinking and clinical judgment to prioritize the patient’s problems and develop a nursing diagnosis.
Choice C: Decide a plan of action
The third step is to decide a plan of action, also known as the planning phase. During this phase, the nurse sets measurable and achievable goals for the patient’s care based on the identified clinical problems. The nurse also develops specific interventions to address these problems and achieve the desired outcomes. This plan serves as a guide for the subsequent implementation phase.
Choice D: Carry out the plan
The fourth step is to carry out the plan, also known as the implementation phase. In this phase, the nurse executes the planned interventions to address the patient’s clinical problems. This may involve administering medications, providing treatments, educating the patient and family, and coordinating care with other healthcare professionals. The nurse continuously monitors the patient’s response to the interventions and makes adjustments as needed.
Choice E: Determine whether the plan was effective
The final step is to determine whether the plan was effective, also known as the evaluation phase. During this phase, the nurse assesses the patient’s progress toward the established goals and evaluates the effectiveness of the interventions. If the desired outcomes are not achieved, the nurse may need to revise the plan and implement new strategies. This ongoing evaluation ensures that the patient’s care is continuously improved and optimized.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
