Which six factors should the nurse consider when choosing a time frame for reassessing the patient’s pain level after implementing pain management?
Agency policy
Type of intervention
Pain severity
If family members are present in the patient’s room
The patient’s psychosocial condition
Risks for adverse effects
Workload of the nurse
The patient’s physical condition
Correct Answer : B,C,E,F,H
Choice A: Agency policy
While agency policy provides guidelines for reassessment intervals, it is not the primary factor in determining the specific time frame for reassessing a patient’s pain level. Policies serve as a general framework, but individual patient needs and clinical judgment should guide the reassessment timing.
Choice B: Type of intervention
This is a correct answer. The type of pain management intervention used significantly influences the reassessment time frame. For example, after administering intravenous pain medication, reassessment should occur sooner compared to oral medications due to the faster onset of action. Different interventions have varying durations of effectiveness, necessitating tailored reassessment intervals.
Choice C: Pain severity
This is another correct answer. The severity of the patient’s pain is a crucial factor in determining reassessment timing. Patients experiencing severe pain may require more frequent reassessments to ensure that pain management strategies are effective and to make timely adjustments if needed.
Choice D: If family members are present in the patient’s room
The presence of family members in the patient’s room is not a primary factor in determining the reassessment time frame. While family members can provide valuable support and information, the focus should remain on the patient’s clinical needs and the effectiveness of pain management interventions.
Choice E: The patient’s psychosocial condition
This is a correct answer. The patient’s psychosocial condition, including their emotional and mental state, can impact their perception of pain and response to pain management. Patients with anxiety, depression, or other psychosocial issues may require more frequent reassessments to address both physical and emotional aspects of pain.
Choice F: Risks for adverse effects
This is also a correct answer. The potential for adverse effects from pain management interventions necessitates careful monitoring and timely reassessment. For instance, opioids carry risks of respiratory depression and sedation, requiring close observation and frequent reassessment to ensure patient safety.
Choice G: Workload of the nurse
While the nurse’s workload can influence the practical aspects of care delivery, it should not dictate the reassessment time frame. Patient needs and clinical priorities should guide reassessment intervals, with workload management being a secondary consideration.
Choice H: The patient’s physical condition
This is the final correct answer. The patient’s overall physical condition, including comorbidities and current health status, affects their response to pain management and the need for reassessment. Patients with complex medical conditions may require more frequent monitoring to ensure effective pain control and to promptly address any complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: True
Chemotherapy drugs work by targeting rapidly dividing cells, a characteristic of cancer cells. However, they cannot selectively distinguish between cancer cells and normal cells that also divide rapidly, such as those in the bone marrow, digestive tract, and hair follicles. This lack of selectivity leads to the common side effects of chemotherapy, such as hair loss, nausea, and decreased blood cell counts. The inability to differentiate between normal and cancer cells is a significant limitation of traditional chemotherapy.
Choice B: False
This choice is incorrect. If chemotherapy drugs could selectively target only cancer cells, the treatment would have fewer side effects and be more effective. However, the non-selective nature of these drugs means they also damage normal, healthy cells that divide rapidly. This non-selectivity is why patients undergoing chemotherapy often experience a range of side effects, as the treatment impacts both cancerous and healthy cells.
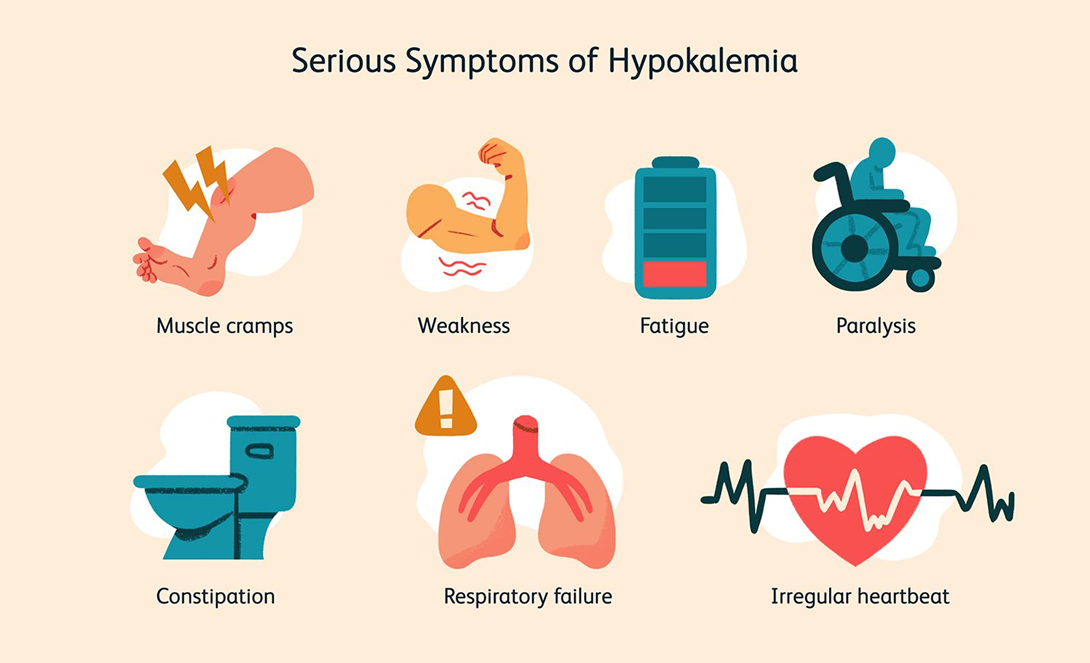
Correct Answer is A
Explanation
Choice A: Infuse the KCl at a maximum rate of 10 mEq/hr
This is the correct answer. The recommended infusion rate for potassium chloride is generally not to exceed 10 mEq per hour to avoid complications such as hyperkalemia and cardiac arrhythmias. This rate ensures that the potassium is administered safely and effectively, allowing for proper monitoring and adjustment if necessary.
Choice B: Discontinue cardiac monitoring during the infusion
This choice is incorrect. Cardiac monitoring is essential during the infusion of potassium chloride, especially in patients with severe hypokalemia, due to the risk of arrhythmias and other cardiac complications. Continuous monitoring allows for the early detection of any adverse effects and timely intervention.
Choice C: Administer the KCl as a rapid IV bolus
Administering potassium chloride as a rapid IV bolus is dangerous and contraindicated. Rapid infusion can lead to severe hyperkalemia, which can cause fatal cardiac arrhythmias. Potassium chloride should always be administered slowly and diluted in an appropriate volume of fluid.
Choice D: Refuse to give the KCl through a peripheral venous line
While central lines are preferred for higher concentrations of potassium chloride due to the risk of irritation and phlebitis, peripheral lines can be used for lower concentrations and slower infusion rates. Refusing to administer potassium chloride through a peripheral line is not necessary if the infusion is properly managed and monitored.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
