The nurse, caring for an infant whose cleft lip was repaired, should include which interventions in the infant's postoperative plan of care? (Select all that apply.).
Petroleum jelly to the suture line.
Elbow restraints.
Supine and side-lying positions.
Mouth irrigations.
Postural drainage.
Correct Answer : A,B,D
The correct answers are choices A, B, and D.
Choice A rationale:
Applying petroleum jelly to the suture line is a necessary intervention in an infant's postoperative plan of care following cleft lip repair. Petroleum jelly helps to keep the suture line moist and prevents it from sticking to clothing or linens. This promotes proper healing and reduces the risk of trauma to the surgical site.
Choice B rationale:
Using elbow restraints is important to prevent the infant from accidentally touching or scratching the surgical site. Infants are not always able to control their movements effectively, and they may inadvertently disrupt the healing process by touching the suture line. Elbow restraints help maintain the integrity of the surgical site.
Choice C rationale:
While positioning is important in the care of a postoperative infant, supine and side-lying positions are not specific interventions related to cleft lip repair. These positions may be used for general comfort and to prevent complications such as aspiration, but they are not directly related to the surgical site.
Choice D rationale:
Mouth irrigations are not typically recommended in the postoperative care of an infant following cleft lip repair. The surgical site is in the area of the lip, not the mouth, so mouth irrigations are not directly relevant to this procedure.
Choice E rationale:
Postural drainage is not a necessary intervention for an infant following cleft lip repair. Postural drainage is a technique used to help clear mucus and secretions from the lungs in patients with respiratory conditions. It is not applicable to the care of an infant recovering from cleft lip surgery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Calcium carbonate is often given with meals to individuals with chronic renal disease, especially those on dialysis. One of the primary purposes is to bind dietary phosphorus in the gastrointestinal tract. In chronic renal disease, the kidneys are less effective at filtering out excess phosphorus from the blood, leading to elevated phosphorus levels (hyperphosphatemia). Elevated phosphorus levels can contribute to bone and mineral disorders in these patients. Calcium carbonate forms insoluble calcium phosphate complexes with dietary phosphorus, preventing its absorption and facilitating its elimination from the body through the feces.
Choice B rationale:
While calcium carbonate can interact with fat-soluble vitamins like vitamin D, the primary reason for administering it to individuals with chronic renal disease is to manage phosphorus levels. Calcium carbonate can bind phosphorus and prevent its absorption, which is particularly important for patients with compromised kidney function.
Choice C rationale:
Stimulating appetite is not a primary purpose of administering calcium carbonate to children with chronic renal disease. The main focus is on managing phosphorus levels and preventing complications associated with hyperphosphatemia.
Choice D rationale:
Preventing vomiting is not a primary purpose of giving calcium carbonate to children with chronic renal disease. Calcium carbonate is typically used to manage phosphorus levels and complications related to hyperphosphatemia in this population.
Correct Answer is A
Explanation
Choice A rationale:
A goiter refers to the enlargement or hypertrophy of the thyroid gland. This can occur due to various reasons, such as iodine deficiency, autoimmune disorders like Hashimoto's thyroiditis, or Graves' disease (which is associated with hyperthyroidism). The thyroid gland produces hormones that regulate metabolism and growth, and when it becomes enlarged, it can lead to visible swelling in the neck.
Choice B rationale:
The posterior pituitary gland is responsible for the release of hormones like vasopressin (antidiuretic hormone) and oxytocin. A goiter is not associated with the posterior pituitary gland. Issues with the posterior pituitary can lead to problems with water balance and uterine contractions, but not thyroid enlargement.
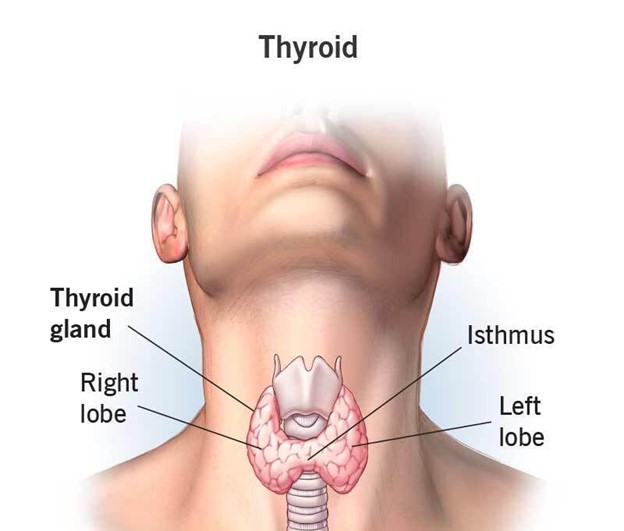
Choice C rationale:
The adrenal glands are responsible for producing hormones like cortisol and adrenaline. While adrenal disorders can lead to various hormonal imbalances, a goiter is not related to adrenal gland function. Adrenal issues might cause symptoms like fatigue, weight changes, and blood pressure irregularities.
Choice D rationale:
The anterior pituitary gland produces hormones that regulate the functions of other endocrine glands, including the thyroid gland. However, a goiter is not directly associated with the anterior pituitary. The anterior pituitary's malfunction can result in disorders like growth hormone deficiency or Cushing's disease, but not thyroid enlargement.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
