The nurse is admitting a client with Abdominal aortic aneurysm. Which assessment data would support the diagnosis?
Shortness of breath.
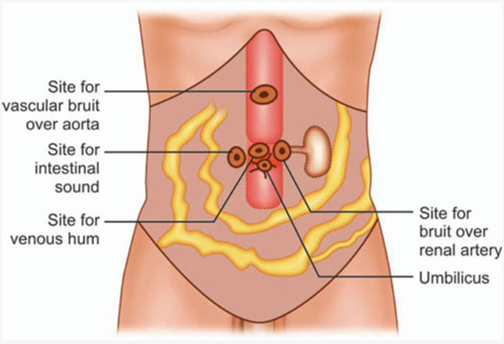
Abdominal bruit.
Ripping abdominal pain.
Decreased urinary output.
The Correct Answer is B
A bruit is a sound that can be heard with a stethoscope when blood flows through a narrowed or damaged artery. An abdominal bruit may indicate an abdominal aortic aneurysm (AAA), which is a bulge or swelling in the main blood vessel that runs from the heart down through the chest and tummy.
Shortness of breath is a common symptom of many conditions, but it is not specific to AAA. It can be caused by heart or lung problems, anemia, anxiety, lack of exercise, obesity, and many other factors. Shortness of breath may occur with a ruptured AAA, but it is not a reliable sign of an intact AAA.
Ripping abdominal pain is a severe and sudden pain that may indicate a ruptured AAA, which is a life-threatening situation that requires immediate medical attention. However, an intact AAA usually does not cause any pain or discomfort. Therefore, ripping abdominal pain is not a good indicator of an AAA diagnosis.
Decreased urinary output is a sign of reduced kidney function, which can have many causes such as dehydration, kidney failure, urinary tract obstruction, or medication side effects. Decreased urinary output is not directly related to AAA, although it may occur as a complication of a ruptured AAA or surgery to repair an AAA.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Maintaining a 2 gram-sodium (salt) diet is an important aspect of managing hypertension. High sodium intake can contribute to elevated blood pressure. Therefore, reducing sodium intake is recommended to help control blood pressure levels. The nurse should provide guidance on reading food labels, avoiding high-sodium processed foods, and incorporating a diet rich in fruits, vegetables, and whole grains.
The other options listed are not appropriate or beneficial for managing hypertension:
Maintaining a low-potassium diet: Potassium is an essential mineral that helps regulate blood pressure. While specific potassium restrictions may be necessary for some individuals with certain medical conditions, most people with hypertension do not need to limit their potassium intake. In fact, a balanced diet with adequate potassium is generally recommended.
Skipping a medication dose if dizziness occurs: It is not advisable to skip medication doses without consulting a healthcare provider. Hypertension medications are prescribed to help control blood pressure, and missing doses can lead to uncontrolled hypertension and potential complications. If the client experiences dizziness or other side effects from the medication, they should consult their healthcare provider for appropriate management.
Drinking three glasses of wine a day: Excessive alcohol consumption can contribute to elevated blood pressure. The recommended alcohol intake for individuals with hypertension is moderate or limited to moderate levels, which typically means no more than one drink per day for women and two drinks per day for men. Drinking excessive amounts of wine or any alcoholic beverage can negatively affect blood pressure control.
Correct Answer is D
Explanation
Among the given findings, the most important finding to report to the health care provider in a client with a hypertensive emergency is the new-onset blurry vision and facial asymmetry. These symptoms may indicate that the client is experiencing a hypertensive crisis with potential complications such as hypertensive encephalopathy or stroke.
Blurred vision and facial asymmetry are concerning neurological symptoms that suggest possible damage to the blood vessels or organs in the brain. It is crucial to notify the health care provider immediately so that appropriate interventions can be initiated to address the underlying cause and prevent further complications.
While the other findings may also be associated with elevated blood pressure, the new-onset blurry vision and facial asymmetry indicate possible neurological involvement and require immediate attention. Headache, epistaxis (nosebleed), and decreased urine output may be significant symptoms, but the potential neurological implications make the new-onset blurry vision and facial asymmetry the priority for reporting.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
