The nurse is caring for a client who is taking diclofenac for rheumatoid arthritis. During a clinic visit, the client appears pale and reports increasing fatigue.
Which of the client’s serum laboratory values is most important for the nurse to review?
Total protein.
Hemoglobin.
Glucose.
Sodium.
The Correct Answer is B
Choice A rationale:
Total protein is a measure of the overall protein content in the blood. It includes albumin and globulin.
While it can be helpful in assessing nutritional status and liver function, it is not directly relevant to the client's current symptoms of pallor and fatigue.
Decreased total protein can indicate malnutrition or liver disease, but these conditions would not typically cause the specific symptoms of pallor and fatigue.
Therefore, total protein is not the most important laboratory value to review in this case.
Choice B rationale:
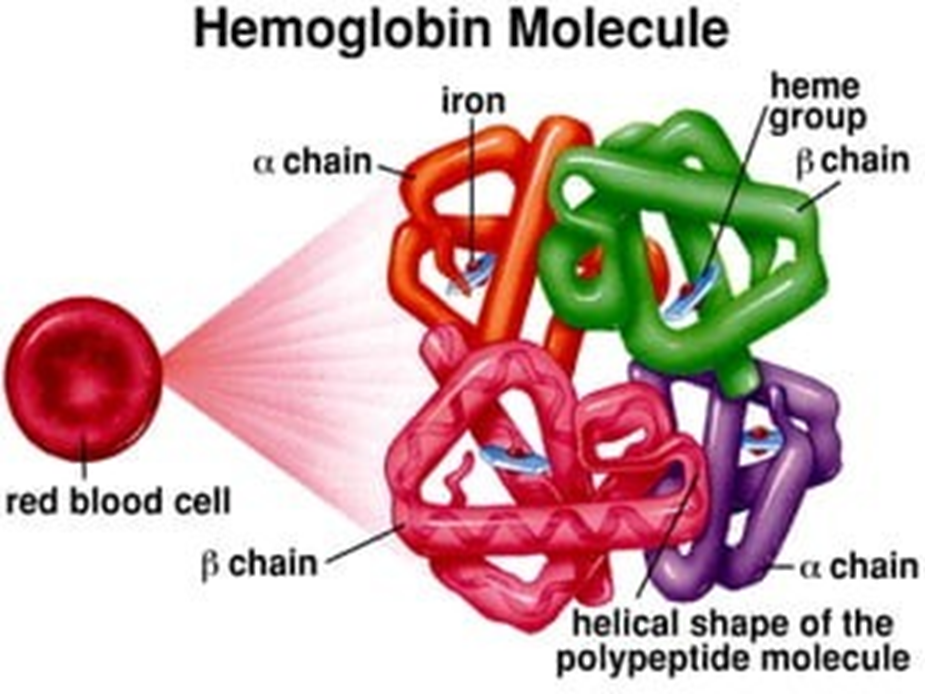
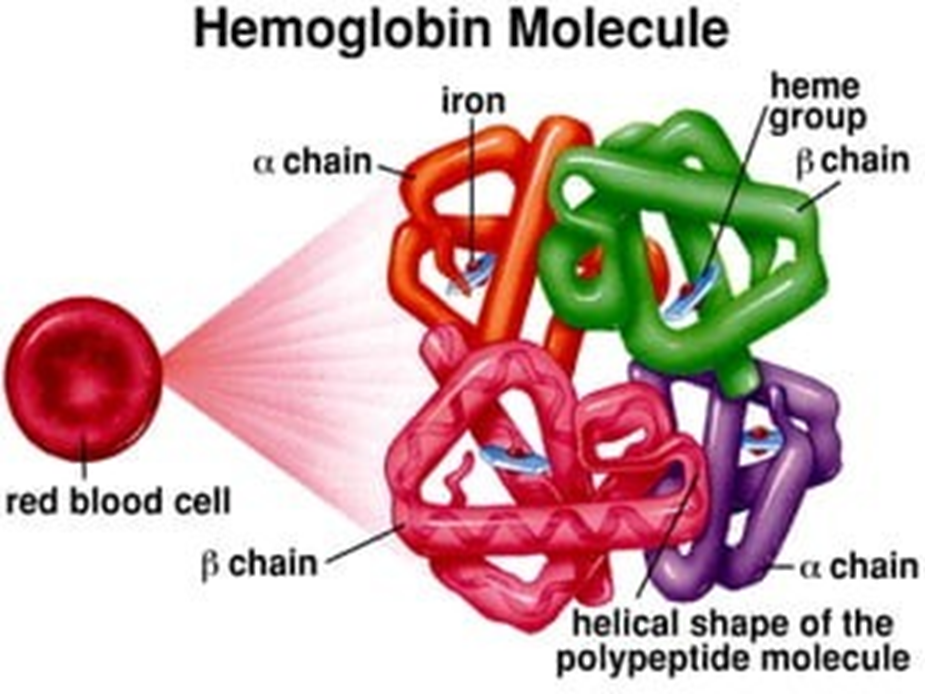
Hemoglobin is the protein in red blood cells that carries oxygen throughout the body.
Paleness (pallor) is a common sign of anemia, which is a condition characterized by a low hemoglobin level. Fatigue is also a common symptom of anemia, as the body's tissues are not receiving enough oxygen.
Diclofenac, a non-steroidal anti-inflammatory drug (NSAID), can cause gastrointestinal bleeding, which can lead to anemia. Therefore, it is essential for the nurse to review the client's hemoglobin level to assess for potential anemia.
Choice C rationale:
Glucose is a type of sugar that the body uses for energy.
Abnormal glucose levels can cause various symptoms, including fatigue. However, glucose levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for diabetes or other disorders that affect glucose metabolism.
Therefore, glucose is not the most likely cause of the client's symptoms.
Choice D rationale:
Sodium is an electrolyte that helps regulate fluid balance in the body.
Abnormal sodium levels can cause various symptoms, including fatigue and weakness. However, sodium levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for electrolyte imbalances. Therefore, sodium is not the most likely cause of the client's symptoms.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A rationale:
Total protein is a measure of the overall protein content in the blood. It includes albumin and globulin.
While it can be helpful in assessing nutritional status and liver function, it is not directly relevant to the client's current symptoms of pallor and fatigue.
Decreased total protein can indicate malnutrition or liver disease, but these conditions would not typically cause the specific symptoms of pallor and fatigue.
Therefore, total protein is not the most important laboratory value to review in this case.
Choice B rationale:
Hemoglobin is the protein in red blood cells that carries oxygen throughout the body.
Paleness (pallor) is a common sign of anemia, which is a condition characterized by a low hemoglobin level. Fatigue is also a common symptom of anemia, as the body's tissues are not receiving enough oxygen.
Diclofenac, a non-steroidal anti-inflammatory drug (NSAID), can cause gastrointestinal bleeding, which can lead to anemia. Therefore, it is essential for the nurse to review the client's hemoglobin level to assess for potential anemia.
Choice C rationale:
Glucose is a type of sugar that the body uses for energy.
Abnormal glucose levels can cause various symptoms, including fatigue. However, glucose levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for diabetes or other disorders that affect glucose metabolism.
Therefore, glucose is not the most likely cause of the client's symptoms.
Choice D rationale:
Sodium is an electrolyte that helps regulate fluid balance in the body.
Abnormal sodium levels can cause various symptoms, including fatigue and weakness. However, sodium levels would not typically cause pallor.
Additionally, there is no indication in the question stem that the client has any risk factors for electrolyte imbalances. Therefore, sodium is not the most likely cause of the client's symptoms.
Correct Answer is B
Explanation
Choice A rationale:
Wild rice is naturally gluten-free. It is not a grain, but rather a semi-aquatic grass seed. It is safe for individuals with celiac disease to consume.
Wild rice is a good source of nutrients. It is high in fiber, protein, and antioxidants, and it contains a variety of vitamins and minerals, including manganese, phosphorus, magnesium, and zinc. These nutrients can help to support overall health and well-being.
Wild rice can be a versatile ingredient in many dishes. It can be used in salads, soups, stews, pilafs, and even desserts.
Choice B rationale:
Oatmeal is not gluten-free. It is made from oats, which are a type of cereal grain that contains gluten. Individuals with celiac disease must avoid gluten, as it can trigger an autoimmune reaction that damages the small intestine.
Even small amounts of gluten can cause harm. Consuming even a small amount of oatmeal can cause symptoms such as abdominal pain, bloating, diarrhea, fatigue, and headache in individuals with celiac disease.
Long-term damage can occur. If individuals with celiac disease continue to consume gluten, it can lead to long-term health problems, such as malnutrition, osteoporosis, and infertility.
Choice C rationale:
Corn chips are typically gluten-free. However, it is important to check the label to be sure, as some brands may contain gluten- containing ingredients, such as wheat flour or barley malt.
Reading labels is essential. Individuals with celiac disease should always read food labels carefully to ensure that products are gluten-free.
Choice D rationale:
Potatoes are naturally gluten-free. They are a safe and healthy food choice for individuals with celiac disease.
Potatoes are a versatile and nutritious food. They are a good source of carbohydrates, fiber, potassium, vitamin C, and other nutrients.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
