The nurse is informed that a newborn infant with Apgar scores of 1 and 4 will be brought to the neonatal intensive care unit (NICU). The nurse determines that which intervention is the priority?
Turning on the apnea and cardiorespiratory monitor.
Connecting the resuscitation bag to oxygen.
Setting up the radiant warmer control temperature at 36.4°C (97.5°F).
Preparing for the insertion of an intravenous (IV) line with D5W.
The Correct Answer is B
Choice A Reason:
Turning on the apnea and cardiorespiratory monitor is important for continuous monitoring of the newborn’s vital signs. However, it is not the immediate priority. The newborn’s low Apgar scores indicate severe distress, and immediate resuscitation efforts are necessary to stabilize the infant.
Choice B Reason:
Connecting the resuscitation bag to oxygen is the priority action. The newborn’s Apgar scores of 1 and 4 suggest significant respiratory and cardiovascular compromise. Providing oxygen and assisting with ventilation are critical to ensure adequate oxygenation and perfusion, which are essential for the infant’s survival.
Choice C Reason:
Setting up the radiant warmer control temperature at 36.4°C (97.5°F) is important for maintaining the newborn’s body temperature. However, this is not the immediate priority. Stabilizing the newborn’s respiratory and cardiovascular status takes precedence over temperature regulation.
Choice D Reason:
Preparing for the insertion of an intravenous (IV) line with D5W is necessary for administering fluids and medications. However, it is not the immediate priority. Ensuring the newborn’s airway, breathing, and circulation are stable is the first step in neonatal resuscitation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason:
Cocaine use is a significant risk factor for placental abruption. Cocaine causes vasoconstriction, which can lead to reduced blood flow to the placenta and increase the risk of abruption. However, while cocaine use is a serious concern, it is not the most common risk factor for placental abruption.
Choice B reason:
Blunt force trauma, such as from a car accident or a fall, can cause placental abruption by physically separating the placenta from the uterine wall. This type of trauma is a recognized risk factor but is less common compared to other factors like hypertension.
Choice C reason:
Hypertension, whether chronic or pregnancy-induced (such as preeclampsia), is the most common risk factor for placental abruption. High blood pressure can damage the blood vessels in the placenta, leading to separation from the uterine wall. This condition is particularly concerning because it can lead to severe complications for both the mother and the fetus, including preterm birth, low birth weight, and stillbirth.
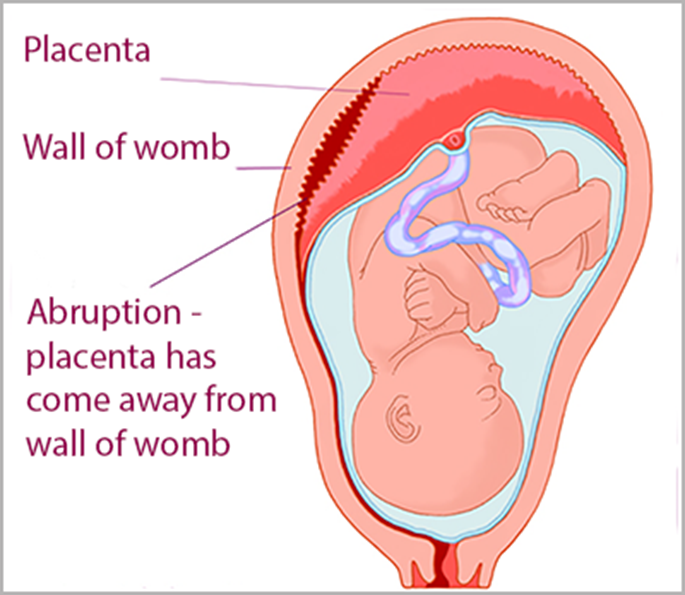
Choice D reason:
Cigarette smoking is another risk factor for placental abruption. Smoking during pregnancy can lead to reduced oxygen supply to the fetus and damage to the placental blood vessels. While it is a significant risk factor, it is not as common as hypertension.
Correct Answer is C
Explanation
Choice A Reason:
Administering oxygen by non-rebreather mask at 5 L/min is a common intervention for patients who may be experiencing respiratory distress or hypoxia. A non-rebreather mask can deliver high concentrations of oxygen, typically between 60% to 90% FiO2, which is crucial in emergency situations such as severe hypoxia, respiratory failure, or carbon monoxide poisoning. Given the client’s stable respiratory rate of 18/min and pulse of 80/min, this prescription does not require immediate clarification.
Choice B Reason:
Obtaining laboratory studies of prothrombin time (PT) and partial thromboplastin time (PTT) is a standard procedure to assess the blood’s clotting ability. These tests are essential for identifying any coagulation disorders, monitoring the effectiveness of anticoagulant therapy, and evaluating the risk of bleeding before surgical procedures. Given the client’s recent delivery and potential for postpartum hemorrhage, this prescription is appropriate and does not require clarification.
Choice C Reason:
Methylergonovine (Methergine) is an ergot alkaloid used to prevent or treat excessive bleeding after childbirth by inducing uterine contractions. However, it is contraindicated in patients with hypertension due to its potential to cause severe vasoconstriction and elevate blood pressure further. The client’s blood pressure is already elevated at 146/94 mm Hg, making this prescription potentially harmful and requiring clarification.
Choice D Reason:
Inserting an indwelling urinary catheter is a common practice in postpartum care to monitor urine output and prevent bladder distention, which can interfere with uterine contraction and increase the risk of postpartum hemorrhage. This intervention is appropriate for the client’s condition and does not require clarification.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
