The nurse is observing a parent holding a preterm infant. The infant is sneezing, yawning, and extending the arms and legs. What action by the nurse is best?
Have the parent fold the infant's arms across the chest.
Encourage the parent to place the infant back in the warmer.
Encourage the parent to do kangaroo care.
Cover the infant with a warm bed blanket.
The Correct Answer is C
Choice a) Have the parent fold the infant's arms across the chest is incorrect because this is not a helpful way to calm a preterm infant. Folding the arms across the chest can restrict the infant's breathing and movement, and may increase their stress and discomfort. Preterm infants need gentle and supportive touch, not restraint or pressure.
Choice b) Encourage the parent to place the infant back in the warmer is incorrect because this is not a necessary or beneficial action for a preterm infant who is showing signs of overstimulation. Placing the infant back in the warmer can interrupt the bonding and attachment process between the parent and the infant, and may make the infant feel more isolated and insecure. Preterm infants need close and frequent contact with their parents, not separation or detachment.
Choice c) Encourage the parent to do kangaroo care is correct because this is an effective and evidence-based method of soothing and stabilizing a preterm infant who is experiencing overstimulation. Kangaroo care is a technique where the parent holds the infant skin-to-skin on their chest, providing warmth, comfort, and security. Kangaroo care can reduce the infant's stress hormones, lower their heart rate and blood pressure, improve their oxygenation and breathing, enhance their growth and development, and strengthen their bond with their parent.
Choice d) Cover the infant with a warm bed blanket is incorrect because this is not a sufficient or optimal way to comfort a preterm infant who is displaying signs of overstimulation. Covering the infant with a warm bed blanket can provide some warmth and protection, but it does not offer the same benefits as kangaroo care. A warm bed blanket cannot mimic the parent's heartbeat, voice, smell, and movement, which are essential for the infant's emotional and physiological well-being. Preterm infants need human touch and interaction, not just physical warmth.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice a) Placenta previa is incorrect because this is a condition where the placenta partially or completely covers the cervix, which can cause painless vaginal bleeding in the third trimester. It is not related to trauma and does not require hospitalization unless bleeding occurs.
Choice b) Dehydration is incorrect because this is a condition where the body loses more fluid than it takes in, which can cause symptoms such as thirst, dry mouth, headache, fatigue, and dizziness. It is not a complication of pregnancy and can be prevented by drinking enough water and avoiding caffeine and alcohol.
Choice c) Gestational hypertension is incorrect because this is a condition where the blood pressure rises above 140/90 mmHg after 20 weeks of pregnancy, which can cause complications such as preeclampsia, eclampsia, and fetal growth restriction. It is not caused by trauma and can be managed by regular antenatal care and medication if needed.
Choice d) Abruptio placentae is correct because this is a condition where the placenta separates from the uterine wall before delivery, which can cause severe vaginal bleeding, abdominal pain, uterine contractions, and fetal distress. It is a life-threatening emergency that can be triggered by trauma and requires immediate delivery of the baby and treatment of shock and blood loss. Therefore, a woman who is 8 months pregnant and involved in a serious motor vehicle crash should be admitted to the hospital for observation for this complication.
Correct Answer is C
Explanation
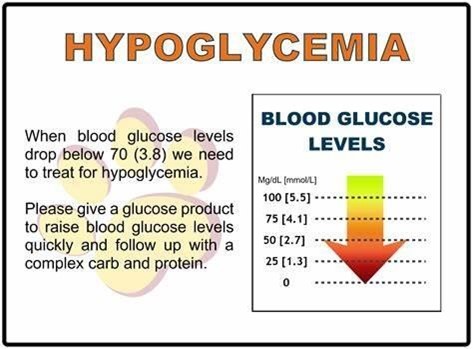
Choice a) D5W intravenously is incorrect because this is not the preferred method of feeding for a hypoglycemic infant. D5W stands for dextrose 5% in water, which is a solution that contains glucose and water. It can be used to treat hypoglycemia by providing a source of energy and fluid to the infant. However, it has several disadvantages, such as requiring an invasive procedure, increasing the risk of infection, causing fluid overload or electrolyte imbalance, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, D5W intravenously should be reserved for severe cases of hypoglycemia that do not respond to oral or enteral feeding.
Choice b) Formula via nasogastric tube is incorrect because this is not the first-line option of feeding for a hypoglycemic infant. Formula is an artificial substitute for breast milk that contains nutrients and calories to support the infant's growth and development. It can be given via nasogastric tube, which is a tube that passes through the nose and into the stomach, when the infant cannot suck or swallow effectively. However, formula has several disadvantages, such as being less digestible, less immunogenic, and less adaptable than breast milk, as well as increasing the risk of necrotizing enterocolitis, allergy, or infection. Therefore, formula via nasogastric tube should be used only when breast milk is unavailable or contraindicated.
Choice c) Breast milk is correct because this is the best and most recommended type of feeding for a hypoglycemic infant. Breast milk is the natural and optimal food for infants that contains all the nutrients and antibodies they need to grow and thrive. It can be given directly from the breast or expressed and fed by bottle or cup. Breast milk has several advantages, such as being easily digestible, enhancing immune function, promoting bonding, and adjusting to the infant's needs. Breast milk also contains lactose, which is a natural sugar that can raise the blood glucose level of the infant without causing a spike in insulin secretion. Therefore, breast milk should be offered to the hypoglycemic infant as soon as possible after birth and at regular intervals thereafter.
Choice d) Glucose water in a bottle is incorrect because this is not an appropriate type of feeding for a hypoglycemic infant. Glucose water is a solution that contains glucose and water. It can be given by bottle or cup to provide a quick source of energy to the infant. However, it has several disadvantages, such as providing no other nutrients or calories, interfering with breastfeeding, causing diarrhea or dehydration, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, glucose water in a bottle should be avoided or used sparingly for mild cases of hypoglycemia that do not respond to breast milk.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
