A nurse in a hospital is caring for a client who is at 38 weeks of gestation and has a large amount of painless, bright red vaginal bleeding. The client is placed on a fetal monitor indicating a regular fetal heart rate of 138/min and no uterine contractions. The client's vital signs are: blood pressure 98/52 mm Hg, heart rate 118/min, respiratory rate 24/min, and temperature 36.4°C (97.6°F). Which of the following is the priority nursing action?
Insert an indwelling urinary catheter.
Prepare the abdominal and perineal areas.
Witness the signature for informed consent for surgery.
Initiate IV access.
The Correct Answer is D
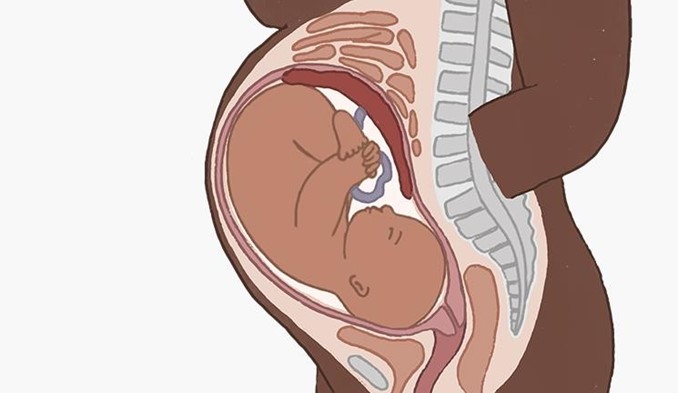
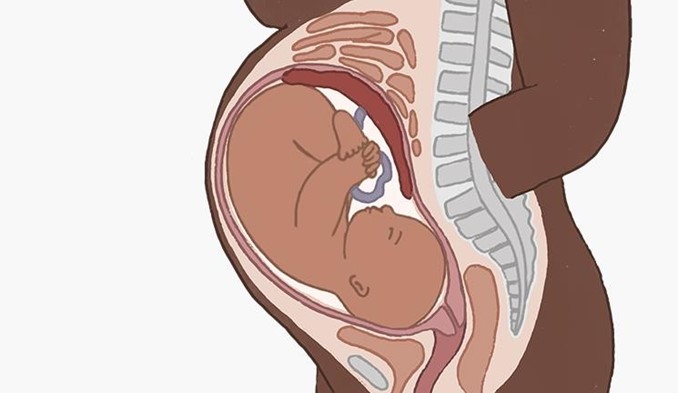
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A) Increased urinary output: This is not a sign of sepsis in newborns. In fact, sepsis can cause reduced urinary output due to poor blood flow to the kidneys and dehydration.
Choice B) Hypothermia: This is a sign of sepsis in newborns. Sepsis can cause changes in temperature, often fever, but sometimes low temperature. Hypothermia can indicate a severe infection that affects the body's ability to regulate its temperature.
Choice C) Wakefulness: This is not a sign of sepsis in newborns. Sepsis can cause reduced activity and lethargy due to inflammation and organ dysfunction.
Choice D) Interest in feeding: This is not a sign of sepsis in newborns. Sepsis can cause reduced sucking and difficulty feeding due to poor appetite, nausea, vomiting, and abdominal distension.
Correct Answer is D
Explanation
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
