We become concerned about the presence of Spinal Bifida when we note
The Correct Answer is {"dropdown-group-1":"D"}
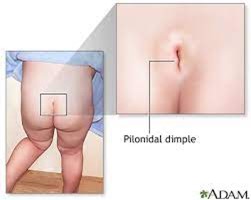
Pilonidal dimpling with the presence of an abnormal tuft of hair in or near the dimple
Explanation:
Spina bifida is a congenital condition where there is incomplete closing of the backbone and membranes around the spinal cord during early development in the womb. Pilonidal dimpling with the presence of an abnormal tuft of hair in or near the dimple is a specific sign of spina bifida. This condition is called "sacral dimple," and it can indicate an underlying issue with the spinal cord and nerves. An abnormal tuft of hair in or near the dimple suggests a neural tube defect, which is characteristic of spina bifida.
Why the other choices are incorrect:
A. complete paralysis:
Complete paralysis is a severe neurological symptom but it is not specific to spina bifida. It can occur due to various other conditions as well, such as spinal cord injuries, infections, and neurological disorders. It's not a characteristic sign of spina bifida.
B. Petechiae:
Petechiae are small, red or purple spots on the skin that are caused by bleeding under the skin. They are usually associated with bleeding disorders, infections, or other medical conditions. Petechiae are not a characteristic sign of spina bifida.
C. Abnormal Vital Signs:
While spina bifida can potentially lead to neurological complications that might influence vital signs, the presence of abnormal vital signs is a non-specific symptom. Abnormal vital signs could be caused by a wide range of medical conditions, and they are not directly indicative of spina bifida.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
A. Replacement therapy may require daily subcutaneous injections.
Explanation: Growth hormone deficiency (hypopituitarism) often requires treatment with growth hormone therapy. One common method of administering growth hormone is through daily subcutaneous injections. Subcutaneous injections involve injecting the medication under the skin into the fatty tissue. This is a routine part of growth hormone therapy, and nursing considerations would include educating the child and their family about proper injection techniques, site rotation, and adherence to the treatment schedule.
Explanation for the other choices:
B. Lifelong replacement therapy will be required:
This statement is generally true. Growth hormone deficiency often requires long-term treatment, which may extend throughout childhood and adolescence. However, in some cases, the need for growth hormone therapy might change based on the individual's response to treatment and growth patterns.
C. Treatment is most successful if started during adolescence:
The optimal timing for starting growth hormone therapy can vary depending on the specific circumstances and the underlying cause of growth hormone deficiency. While treatment during adolescence can be effective, growth hormone therapy can also be successful if started earlier in childhood or later in adolescence. The key is identifying and treating the deficiency as soon as possible to promote healthy growth.
D. Treatment is considered successful if children attain full stature by adulthood:
While growth hormone therapy aims to support growth, achieving "full stature" might not always be possible. The goal of treatment is to help the child reach a more typical height based on their genetic potential and individual response to therapy. The success of treatment is determined by improvements in growth velocity and height, rather than necessarily achieving "full stature," which can vary greatly among individuals.
Correct Answer is B
Explanation
A) Low-protein, low-potassium diet:
While low-protein and low-potassium diets can be appropriate for certain kidney conditions, such as chronic kidney disease, they are not typically the primary focus in the acute phase of glomerulonephritis. Protein restriction might be considered if there is significant kidney damage, and potassium levels are elevated.
B) Low-sodium fluid-restricted diet:
This is the most appropriate option. In acute glomerulonephritis, the kidneys' ability to regulate sodium and fluid balance may be impaired due to inflammation and decreased glomerular filtration. Fluid retention and peripheral edema are common. A low-sodium diet helps reduce fluid retention and manage edema.
C) Low carbohydrate, low-protein diet:
Low-carbohydrate and low-protein diets are not the main dietary considerations for acute glomerulonephritis. The primary focus is on managing sodium and fluid intake due to impaired kidney function.
D) Regular diet, no added salt:
A regular diet without added salt might exacerbate the fluid retention and edema associated with acute glomerulonephritis. Sodium intake needs to be controlled to prevent further fluid buildup.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
