What action by the nurse is the most important action in preventing neonatal infection?
Standard Precautions
Good hand hygiene
Separate gown technique
Isolation of infected infants
The Correct Answer is B
Choice A: This is incorrect because Standard Precautions are a set of guidelines that apply to all patients, regardless of their infection status. They include using personal protective equipment, handling sharps and waste properly, and cleaning and disinfecting equipment and surfaces. However, they are not enough to prevent neonatal infection, as some pathogens can still be transmitted by contact or droplet.
Choice B: This is the correct answer because good hand hygiene is the most effective way to prevent the transmission of microorganisms that can cause neonatal infection. The nurse should wash their hands with soap and water or use an alcohol-based hand rub before and after touching the infant, the infant's environment, or any items that come in contact with the infant. The nurse should also educate the parents and visitors on the importance of hand hygiene and how to perform it correctly.
Choice C: This is incorrect because a separate gown technique involves wearing a clean gown for each infant and discarding it after use. This can help prevent cross-contamination between infants, but it does not eliminate the need for hand hygiene. The nurse should still wash their hands before and after wearing a gown, as well as before and after touching the infant or any items that come in contact with the infant.
Choice D: This is incorrect because isolation of infected infants involves placing them in a separate room or area with restricted access and using additional precautions based on the mode of transmission of the infection. This can help prevent the spread of infection to other infants, staff, or visitors, but it does not eliminate the need for hand hygiene. The nurse should still wash their hands before and after entering and leaving the isolation area, as well as before and after touching the infant or any items that come in contact with the infant.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
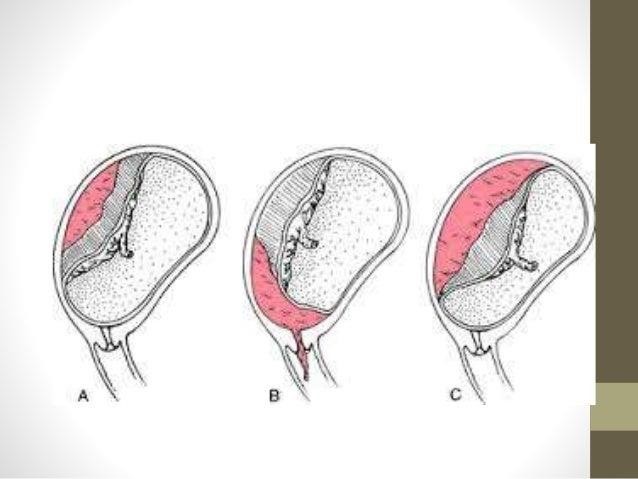
Choice a) This could result in profound bleeding is correct because this is the primary reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination involves inserting a gloved finger or a speculum into the vagina and cervix to assess their dilation, effacement, position, and station. This can cause trauma to the cervix or the placenta, which can trigger severe hemorrhage and endanger the mother and the fetus. Therefore, this explanation is accurate and appropriate.
Choice b) This could initiate preterm labor is incorrect because this is not the main reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may stimulate uterine contractions, which can lead to preterm labor and delivery. However, this is not the most serious or likely complication of an internal examination for a client who has placenta previa, as the bleeding risk is much higher and more urgent. Therefore, this explanation is incomplete and misleading.
Choice c) There is an increased risk of introducing infection is incorrect because this is not a specific reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may introduce bacteria or other microorganisms into the vagina or cervix, which can cause infection and inflammation. However, this is a general risk that applies to any pregnant woman who undergoes an internal examination, not just those who have placenta previa. Therefore, this explanation is irrelevant and inaccurate.
Choice d) There is an increased risk of rupture of the membranes is incorrect because this is not a relevant reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may cause rupture of the membranes, which are the sacs that contain the amniotic fluid and the fetus. However, this is not a significant or common complication of an internal examination for a client who has placenta previa, as the membranes are usually located above or away from the placenta and cervix. Therefore, this explanation is improbable and inaccurate.
Correct Answer is B
Explanation
Choice A) "Oh, don't worry about that. It's okay." is incorrect because this is not a helpful or informative response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not explain what the black, sticky stuff in the diaper is, why it is there, or how long it will last. It also does not address the father's concern or curiosity, and may make him feel dismissed or ignored. Therefore, this response is inadequate and inappropriate.
Choice B) "That's meconium, which is your baby's first stool. It's normal." is correct because this is a clear and accurate response for a first-time father who is changing the diaper of his 1-day-old daughter. This response explains what the black, sticky stuff in the diaper is, which is meconium. Meconium is a substance that consists of amniotic fluid, mucus, bile, and other waste products that accumulate in the baby's intestines before birth. It is usually passed within the first 24 to 48 hours after birth, and then replaced by transitional or regular stools. Meconium has a dark green or black color and a thick, sticky consistency. It does not have any odor or bacteria. It is normal and harmless for most babies, unless they inhale it during delivery, which can cause breathing problems or infection. Therefore, this response reassures and educates the father about his baby's condition.
Choice C) "That's transitional stool." is incorrect because this is not a true or complete response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not identify what the black, sticky stuff in the diaper is, which is meconium. Transitional stool is a type of stool that appears after meconium and before regular stools. It usually occurs between the second and fifth day after birth, and then changes to yellow or brown stools. Transitional stool has a greenish-brown color and a loose, seedy consistency. It may have some odor or bacteria. It indicates that the baby's digestive system is maturing and adapting to breast milk or formula. Therefore, this response confuses and misleads the father about his baby's condition.
Choice D) "That means your baby is bleeding internally." is incorrect because this is not a valid or appropriate response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not describe what the black, sticky stuff in the diaper is, which is meconium. Bleeding internally means that blood vessels are damaged or ruptured inside the body, causing blood loss and shock. This can be caused by various factors such as trauma, infection, clotting disorder, or medication. Bleeding internally can manifest as blood in the stool, urine, vomit, or saliva. However, it does not cause black, sticky stools like meconium. Moreover, this response scares and alarms the father without any evidence or reason. Therefore, this response is false and unethical.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
