While assessing the newborn, the nurse should be aware that the average expected apical pulse range of a full-term, quiet, alert newborn is __ beats/min.
100 to 120
120 to 160
80 to 100
150 to 180
The Correct Answer is B
Choice a) 100 to 120 is incorrect because this is too low for a normal newborn's heart rate. The heart rate of a newborn is influenced by factors such as gestational age, activity level, temperature, and health status. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which reflects their high metabolic rate and oxygen demand. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
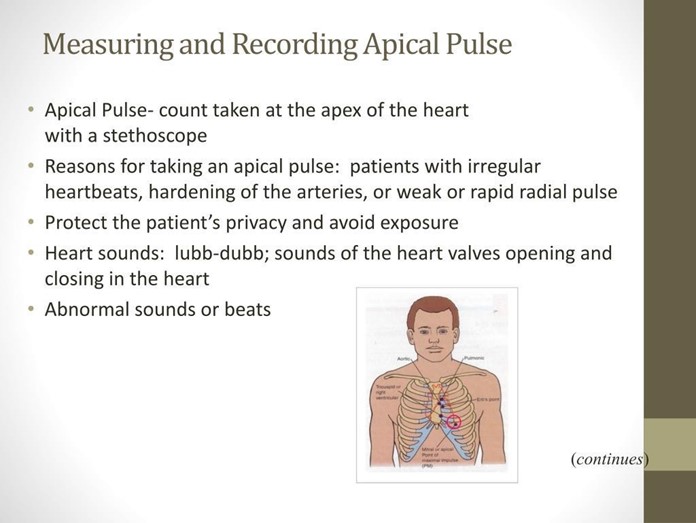
Choice b) 120 to 160 is correct because this is the normal range for a full-term, quiet, alert newborn's heart rate. The apical pulse is the best way to measure the heart rate of a newborn, as it reflects the actual contractions of the heart. The apical pulse can be auscultated at the fourth intercostal space on the left side of the chest, just below the nipple line. The nurse should count the apical pulse for a full minute, as it may vary with the respiratory cycle.
Choice c) 80 to 100 is incorrect because this is also too low for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is higher than that of an adult or an older child. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice d) 150 to 180 is incorrect because this is too high for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is lower than that of a preterm or a crying newborn. A heart rate above 160 beats per minute may indicate tachycardia, which can be caused by fever, infection, anemia, or hyperthyroidism.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A) Wrap the cord loosely with a sterile towel saturated with warm normal saline: This is not an appropriate action because it does not relieve the compression of the cord, which can cause fetal hypoxia and acidosis. The cord should be kept moist, but not wrapped around anything.
Choice B) Place a sterile gloved hand into the vagina and hold the presenting part off the cord while calling for assistance: This is the correct action because it prevents further descent of the fetus and reduces the pressure on the cord, which can improve fetal oxygenation and blood flow. The nurse should also elevate the woman's hips and place her in a knee-chest or Trendelenburg position to reduce gravity. The nurse should call for immediate assistance and prepare for an emergency cesarean section.
Choice C) Increase the IV drip rate: This is not an appropriate action because it does not address the cause of the variable decelerations, which is cord compression. Increasing the IV fluid may cause fluid overload and worsen maternal and fetal outcomes.
Choice D) Administer oxygen to the woman via mask at 8 to 10 L/minute: This is not an appropriate action because it does not relieve the cord compression, which is the main threat to fetal well-being. Oxygen administration may be helpful in some cases of fetal distress, but it is not sufficient in this situation.
Correct Answer is A
Explanation
Choice A) Maternal blood type is correct because this is an essential and relevant information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Spontaneous abortion, also known as miscarriage, is the loss of pregnancy before 20 weeks of gestation. It can be caused by various factors such as chromosomal abnormalities, infections, trauma, or hormonal imbalances. Maternal blood type is the classification of blood based on the presence or absence of antigens and antibodies on the red blood cells and plasma. The most common blood types are A, B, AB, and O, and each can be positive or negative for the Rh factor. Checking maternal blood type can help to identify and prevent Rh incompatibility, which is a condition that occurs when the mother has Rh-negative blood and the fetus has Rh-positive blood. This can cause the mother's immune system to produce antibodies that attack the fetal red blood cells, leading to hemolytic disease of the fetus and newborn (HDFN), which can cause anemia, jaundice, or death. To prevent this, the nurse should administer Rh immunoglobulin (RhoGAM) to the mother within 72 hours after a spontaneous abortion or any event that may cause mixing of maternal and fetal blood. Therefore, this information is vital and appropriate for the nurse to check.
Choice B) Past obstetric history is incorrect because this is not an essential or urgent information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Past obstetric history is the record of previous pregnancies and their outcomes, such as number, duration, complications, or interventions. It can provide useful information for assessing the risk factors and health status of the current pregnancy. However, it does not have any immediate impact or implication for the management of a spontaneous abortion, which is a common and unpredictable event that affects about 10% to 20% of all pregnancies. Therefore, this information can be obtained later or from other sources by the nurse.
Choice C) Maternal varicella titer is incorrect because this is not a relevant or necessary information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Varicella titer is a blood test that measures the level of antibodies against varicella-zoster virus (VZV), which causes chickenpox and shingles. It can indicate whether a person has immunity to VZV or needs vaccination. Checking maternal varicella titer may be important for pregnant women who have not had chickenpox or vaccination before, as VZV infection during pregnancy can cause congenital varicella syndrome (CVS), which can affect the development and function of various organs in the fetus. However, it does not relate to spontaneous abortion, which is not caused by VZV infection or immunity. Therefore, this information is irrelevant and unnecessary for the nurse to check.
Choice D) Cervical patency is incorrect because this is not a reliable or accurate information for the nurse to check for a woman who has had a first trimester spontaneous abortion. Cervical patency means how open or closed the cervix is, which can affect the progress and outcome of labor and delivery. The cervix is usually closed and firm during pregnancy, but it gradually softens, shortens, and dilates as labor approaches. Checking cervical patency can help to determine if labor has started or if there are any complications such as preterm labor or cervical incompetence.
However, it does not indicate if a spontaneous abortion has occurred or not, as the cervix may remain closed or partially open after a miscarriage. Moreover, checking cervical patency can be invasive and uncomfortable for the woman who has had a spontaneous abortion, and it may increase the risk of infection or bleeding. Therefore, this information should be checked only when indicated by the physician and with caution by the nurse.

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
