Which actions should the practical nurse (PN) include when assessing a client for signs and symptoms of fluid volume excess? (Select all that apply.)
Palpate the rate and volume of the pulse.
Check fingernails for the presence of clubbing.
Measure body weight at the same time daily
Observe the color and amount of urine
Compare muscle strength of both arms.
Correct Answer : A,C,D
The PN should palpate the rate and volume of the pulse, measure body weight at the same time daily, and observe the color and amount of urine when assessing a client for signs and symptoms of fluid volume excess. These actions can help detect changes in the cardiovascular, renal, and fluid balance systems that may indicate fluid overload, such as tachycardia, bounding pulse, weight gain, edema, oliguria, or dark urine.
The other options are not correct because:
b. Checking fingernails for the presence of clubbing is not relevant for assessing fluid volume excess, as clubbing is a sign of chronic hypoxia or lung disease that causes enlargement of the fingertips and nails.
e. Comparing muscle strength of both arms is not relevant for assessing fluid volume excess, as muscle weakness is not a specific sign of fluid overload, but may be caused by various factors such as electrolyte imbalance, nerve damage, or fatigue.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Explaining the procedure and obtaining the signature is the provider’s responsibility, not the practical nurse’s.
B. Checking the medical record for a signed consent form is part of the practical nurse’s verification role but does not address assessing client understanding.
C. Obtaining consent from a family member is only appropriate if the client is unable to provide it; otherwise, consent must come directly from the client.
D. The practical nurse is responsible for ensuring the client understands the procedure and the purpose of the consent form, reinforcing the provider’s explanation and promoting informed consent.
Correct Answer is A
Explanation
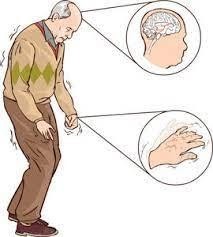
A) Correct- Clients with Parkinson's disease often experience bradykinesia and impaired mobility. Rising slowly from a seated position is important to prevent falls and maintain stability. Affirming the correct movement strategy promotes the client's safety.
B) Incorrect- Telling the UAP to make the client move more quickly could be unsafe and not appropriate for a client with Parkinson's disease. Rapid movements might lead to balance issues or falls.
C) Incorrect- While demonstrating proper technique might be helpful, it's not the most immediate action the nurse should take. The client's safety and well-being are the priority.
D) Incorrect- Painful movement is not the primary issue here. The client's movement is slow due to Parkinson's disease, and this is expected.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
