Which of the following is an appropriate technique for specimen collection?
Performing a heel stick on a 5-year-old patient
Performing a finger stick on a toddler patient
Performing a thumb stick on an infant
Performing a thumb stick on a 5-year-old patient
The Correct Answer is B
Choice A reason:
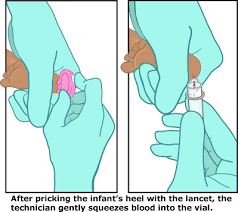
Performing a heel stick on a 5-year-old patient is not an appropriate technique. Heel sticks are typically used for infants, particularly newborns, to minimize discomfort and because their finger pads may not be fully developed for finger sticks. By the age of 5, a child's veins are usually developed enough for venipuncture, which is the preferred method.
Choice B reason:
Performing a finger stick on a toddler patient is an appropriate technique for specimen collection. This method is commonly used for children who are not yet old enough for venipuncture but have outgrown the heel stick method. The finger stick is performed on the palmar surface of the distal phalanx, usually of the middle or ring finger, and is considered safe and effective for collecting small blood samples in toddlers.
Choice C reason:
Performing a thumb stick on an infant is not an appropriate technique. The thumb has a pulse and is more sensitive, which can cause unnecessary pain and distress to the infant. Additionally, the thumb's size and increased movement make it a less suitable site for specimen collection in infants.
Choice D reason:
Performing a thumb stick on a 5-year-old patient is also not an appropriate technique. As with infants, the thumb's sensitivity and the presence of a pulse make it a less desirable site for blood collection. For a 5-year-old, venipuncture or a finger stick on a non-thumb finger would be more appropriate and less distressing.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Notifying the provider about the error is an important step, but it does not correct the error in the patient's chart. Communication with the provider ensures that they are aware of the mistake and can make informed decisions regarding patient care. However, the physical correction of the documentation is also necessary to maintain accurate medical records.
Choice B Reason:
Asking an administrator to erase the error is not a recommended practice. Erasing or using correction fluid can make the chart appear tampered with, which can have legal implications. It is essential that the original entry remains visible to preserve the integrity of the medical record.
Choice C Reason:
Striking a line through the error and initialing is the correct method for correcting a written error in a patient's chart¹². This approach allows the original entry to remain legible, which is crucial for legal and clinical reasons. It also shows that the correction was made by an authorized individual, as the initials indicate who made the change.
Choice D Reason:
Erasing the error and entering the correct information is not an acceptable practice for the same reasons as choice B. It is important not to remove or conceal the original entry, as this could be considered falsifying medical records.
Correct Answer is A
Explanation
Choice A reason:
Reporting the exposure to the supervisor is the immediate and required action after experiencing a needlestick injury. The supervisor will then guide the phlebotomist through the institution's post-exposure protocol, which includes immediate care of the wound, evaluation of the exposure, and initiation of post-exposure prophylaxis (PEP) if necessary. This step is crucial to ensure that the risk of HIV transmission is minimized and that the phlebotomist receives appropriate medical attention and follow-up.
Choice B reason:
Reporting the exposure to the Centers for Disease Control and Prevention (CDC) is not the immediate action required. The CDC provides guidelines and recommendations for handling such incidents, but the initial report and response are managed at the healthcare facility level. The CDC may be involved in the tracking of such incidents on a larger scale or providing statistical data, but they are not the first point of contact.
Choice C reason:
Sending the patient for further sexually transmitted infection (STI) testing is not an immediate action required following a needlestick injury. The patient's HIV status is already known, and the focus should be on the treatment and protection of the healthcare worker who experienced the needlestick. Any additional testing of the patient would be unrelated to the immediate management of the injury.
Choice D reason:
Saving the collection device for future evaluation is not a standard procedure. While the device may be retained as part of the incident investigation to determine how the injury occurred and to improve safety measures, the immediate concern is the treatment of the injured healthcare worker. The device itself does not play a role in the post-exposure management of the worker.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
