Which of the following would be essential to implement to prevent late postpartum hemorrhage? Select one:
Inspecting the placenta after delivery for intactness.
Manually removing the placenta at delivery.
Administering broad-spectrum antibiotics prophylactically.
Applying traction on the umbilical cord to speed up separation of the placenta.
The Correct Answer is A
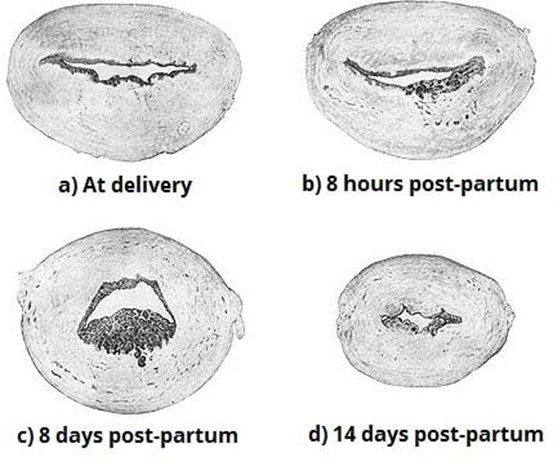
Choice A Reason: Inspecting the placenta after delivery for intactness. This is because inspecting the placenta after delivery for intactness is a nursing intervention that can prevent late postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs more than 24 hours but less than 12 weeks after delivery. Late postpartum hemorrhage can be caused by retained placental fragments, subinvolution of the uterus, infection, or coagulation disorders. Inspecting the placenta after delivery for intactness can help identify and remove any retained placental fragments that may interfere with uterine contraction and involution, which are essential for hemostasis.
Choice B Reason: Manually removing the placenta at delivery. This is an incorrect answer that indicates an inappropriate and risky intervention that can cause late postpartum hemorrhage. Manually removing the placenta at delivery is a procedure that involves inserting a hand into the uterus and detaching the placenta from the uterine wall. Manually removing the placenta at delivery is indicated only for a retained or adherent placenta that does not separate spontaneously or with gentle traction within 30 minutes after delivery. Manually removing the placenta at delivery can cause trauma, infection, or incomplete removal of the placenta, which can increase the risk of late postpartum hemorrhage.
Choice C Reason: Administering broad-spectrum antibiotics prophylactically. This is an incorrect answer that suggests an unnecessary and ineffective intervention that can prevent late postpartum hemorrhage. Administering broad- spectrum antibiotics prophylactically is a pharmacological intervention that involves giving antibiotics to prevent or treat infection. Administering broad-spectrum antibiotics prophylactically is indicated for women with risk factors or signs of infection during or after delivery, such as prolonged rupture of membranes, chorioamnionitis, fever, or foul- smelling lochia. Administering broad-spectrum antibiotics prophylactically may reduce the risk of infection-related late postpartum hemorrhage, but it does not address other causes of late postpartum hemorrhage such as retained placental fragments or subinvolution of the uterus.
Choice D Reason: Applying traction on the umbilical cord to speed up separation of the placenta. This is an incorrect answer that refers to a different intervention that can prevent early postpartum hemorrhage, not late postpartum hemorrhage. Applying traction on the umbilical cord to speed up separation of the placenta is a technique that involves pulling on the umbilical cord while applying counter pressure on the uterus to facilitate placental expulsion. Applying traction on the umbilical cord to speed up separation of the placenta is indicated for active management of the third stage of labor, which can prevent early postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs within 24 hours after delivery. Early postpartum hemorrhage can be caused by uterine atony, retained placenta, lacerations, or coagulation disorders.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
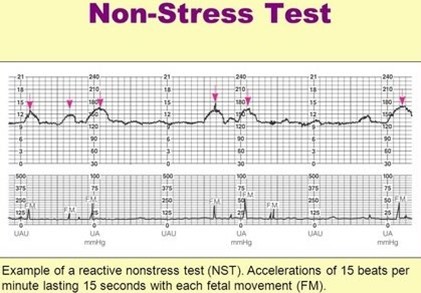
Choice A Reason: A fetal heart rate baseline of 140 with one acceleration to 155 for 15 seconds within 30 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. A non-reactive NST may suggest fetal hypoxia, distress, or sleep, but it does not necessarily indicate a problem. A non-reactive NST may require further testing or stimulation to elicit a reactive result.
Choice B Reason A fetal heart rate baseline of 140 with two accelerations to 160 for 15 seconds within 20 minutes. This is because this strip meets the criteria for a reactive NST, which is a non-invasive test that evaluates fetal well- being and oxygenation by measuring the fetal heart rate response to fetal movements. A reactive NST is defined as having at least two accelerations of the fetal heart rate that are at least 15 beats per minute above the baseline and last for at least 15 seconds within a 20-minute period.
Choice C Reason: A fetal heart rate baseline of 130 with two accelerations to 135 for 15 seconds within 20 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. The accelerations in this strip are not sufficient in amplitude, as they are only 5 beats per minute above the baseline, instead of at least 15 beats per minute.
Choice D Reason: A fetal heart rate baseline of 150 with two accelerations to 160 for 10 seconds within 20 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. The accelerations in this strip are not sufficient in duration, as they last only for 10 seconds, instead of at least 15 seconds.
Correct Answer is B
Explanation
Choice A Reason: "If I try to talk to my partner during a contraction, I can't." This is an incorrect answer that indicates a sign of true labor, not false labor. True labor is a condition where there are regular and painful uterine contractions that cause cervical dilation and effacement, and lead to delivery of the baby and placenta. True labor contractions are usually strong and consistent, and they tend to increase or persist with activity or position changes. True labor contractions can be so intense that they interfere with speech or breathing.
Choice B Reason: ) "My contractions slow down when I walk around." This is because this statement by the client would lead the nurse to suspect that the woman is experiencing false labor, which is also known as Braxton Hicks contractions or practice contractions. False labor is a condition where there are irregular and painless uterine contractions that do not cause cervical dilation or effacement. False labor can occur throughout pregnancy, but it becomes more noticeable and frequent in late pregnancy. False labor contractions are usually weak and inconsistent, and they tend to decrease or stop with activity or position changes.
Choice C Reason: "I feel contractions start mostly in my back and they sweep around to the top of my abdomen." This is an incorrect answer that indicates a sign of true labor, not false labor. True labor contractions usually start in the lower back and radiate to the lower abdomen or groin, following a wave-like patern. False labor contractions are more likely to be felt in the upper abdomen or sides, without a clear patern.
Choice D Reason: "My contractions are about 6 minutes apart and regular." This is an incorrect answer that indicates a sign of true labor, not false labor. True labor contractions usually have a regular frequency and duration, and they become closer and longer as labor progresses. False labor contractions are more likely to have an irregular frequency and duration, and they do not change significantly over time.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
