Medical surgical Exam 1
ATI Medical surgical Exam 1
Total Questions : 82
Showing 10 questions Sign up for moreWhich of the following is the most common risk factor for emphysema?
Explanation
Choice A Reason:
Smoking tobacco is the primary and most significant risk factor for emphysema. Tobacco smoke contains harmful chemicals and toxins that directly damage the lungs. Chronic exposure to cigarette smoke leads to inflammation and destruction of lung tissue, particularly the alveoli, contributing to the development of emphysema.
Choice B Reason:
Between 20 to 30 years of age. While smoking at any age is harmful to lung health, the risk of developing emphysema increases with prolonged exposure to tobacco smoke over many years. Emphysema is typically a disease of middle to older age, with symptoms often appearing after years of smoking.
Choice C Reason:
Asthma is a chronic inflammatory condition of the airways characterized by reversible airflow obstruction and airway hyperresponsiveness. While asthma and emphysema are both respiratory diseases, they have distinct pathophysiological mechanisms and risk factors. Asthma is not a direct cause of emphysema, although some individuals with poorly controlled asthma may develop chronic obstructive pulmonary disease (COPD), which includes emphysema as one of its components.
Choice D Reason:
Pollution is not correct. Environmental pollution, including air pollution from industrial emissions, vehicle exhaust, and particulate matter, can contribute to respiratory problems and exacerbate pre-existing lung conditions. While exposure to pollution can worsen respiratory symptoms and lung function, it is not the primary cause of emphysema. However, long-term exposure to certain pollutants may increase the risk of developing respiratory diseases, including COPD, which encompasses emphysema.

A nurse is providing discharge information to a client who has Parkinson's disease and their family members. Which of the following instructions should the nurse include in the discharge information?
(Select All that Apply.)
Explanation
Choice A Reason:
Encouraging the client to walk regularly is appropriate. Regular exercise, including walking, can help improve mobility, balance, and overall physical function in individuals with Parkinson's disease. It can also help alleviate symptoms such as stiffness and tremors.
Choice B Reason:
Providing the client with fresh fruits and vegetables is appropriate. A healthy diet rich in fresh fruits and vegetables provides essential nutrients, antioxidants, and fiber, which can support overall health and well-being. While diet alone does not directly treat Parkinson's disease, maintaining a nutritious diet is important for overall health.
Choice C Reason:
Restricting fluids to 800 mL/day is inappropriate. Fluid restriction is not typically indicated for individuals with Parkinson's disease unless they have a specific medical condition such as heart failure or kidney disease, which may require fluid restriction as part of their management plan. Restricting fluids excessively can lead to dehydration, which can worsen symptoms such as fatigue, confusion, and constipation, common in Parkinson's disease. Adequate hydration is important for overall health and well-being, including maintaining proper kidney function and preventing urinary tract infections, which individuals with Parkinson's disease may be susceptible to due to urinary retention issues.
Choice D Reason:
Minimizing exposure to outside activities is inappropriate. While it's important for individuals with Parkinson's disease to take precautions to avoid falls and injuries, completely restricting exposure to outside activities is not necessary or advisable. Physical activity, social engagement, and exposure to sunlight are beneficial for both physical and mental health. Encouraging individuals with Parkinson's disease to remain engaged in activities they enjoy, with appropriate safety measures in place, can help maintain their quality of life and overall well-being.
Choice E Reason:
Teaching the client how to use a walker is inappropriate. Assistive devices such as walkers can help individuals with Parkinson's disease maintain mobility and independence, especially if they experience gait disturbances or balance problems. Teaching the client how to use a walker safely and effectively can enhance their quality of life and reduce the risk of falls.
A nurse is providing discharge instructions to a client who has epilepsy. Which of the following instructions should be included in the nurse's teaching?
(Select All that Apply.)
Explanation
Choice A Reason:
Refraining from climbing ladders is appropriate. Climbing ladders involves a risk of falling, which can be particularly hazardous for individuals with epilepsy. Seizures can occur unexpectedly and may cause loss of muscle control or consciousness, increasing the risk of falls from heights such as ladders. Falling from a ladder during a seizure can result in serious injuries, including head trauma, fractures, or other injuries from impact. Advising the client to refrain from climbing ladders helps mitigate the risk of falls and associated injuries during a seizure episode, promoting their safety and well-being.
Choice B Reason:
Do not go swimming without a partner is inappropriate. Swimming alone can be dangerous for individuals with epilepsy as they may be at risk of drowning if they experience a seizure while in the water. Having a swimming partner can provide assistance and ensure safety in case of a seizure.
Choice C Reason:
Refraining from driving unless seizure-free for 3 months is appropriate. Driving restrictions are often recommended for individuals with epilepsy to minimize the risk of accidents caused by seizures. Many jurisdictions require individuals with epilepsy to be seizure-free for a certain period, typically around 3 to 6 months, before resuming driving.
Choice D Reason:
Avoiding using power tools is appropriate. Operating power tools or machinery can be hazardous if a seizure occurs, potentially leading to serious injuries. Therefore, individuals with epilepsy should avoid using power tools to reduce the risk of accidents during a seizure.
Choice E Reason:
Placing client on the floor when having a seizure is appropriate. Placing the client on the floor during a seizure helps prevent injury from falls. It is safer to have the individual lie down on a flat surface to reduce the risk of head injury or other trauma during the seizure.
Choice F Reason:
Placing client on their back when they are recovering from a seizure appropriate. Placing the client on their back after a seizure helps maintain an open airway and facilitates recovery. This position allows for proper breathing and circulation while monitoring the individual's condition.
A nurse is caring for a client who was involved in a motor vehicle accident. The client is alert and oriented and reports a loss of consciousness immediately after the accident. Which of the following additional manifestations should the nurse assess the client for?
(Select All that Apply.)
Explanation
Choice A Reason:
Pupillary dilation is correct. Pupillary changes can indicate neurological dysfunction following a head injury. Dilated pupils may suggest increased intracranial pressure or damage to specific brain structures.
Choice B Reason:
Persistent headache is correct .Headaches are a common symptom following a head injury. Persistent or worsening headaches can indicate ongoing neurological issues and should be monitored closely.
Choice C Reason:
Presence of hand tremors is incorrect. Hand tremors are not typically associated with loss of consciousness following a motor vehicle accident. While hand tremors can occur in various conditions, such as essential tremor or Parkinson's disease, they are not typically a direct manifestation of a head injury. The primary concern immediately following a motor vehicle accident with loss of consciousness is assessing for signs of neurological dysfunction, such as altered level of consciousness, pupillary changes, and persistent headache. Hand tremors may be assessed in other contexts, but they are not directly related to the immediate assessment of a client following a motor vehicle accident with loss of consciousness.
Choice D Reason:
Difficulty waking is correct. Difficulty waking or altered level of consciousness can indicate neurological impairment and may be indicative of a concussion or other brain injury.
E. Foot drop is incorrect. Foot drop refers to difficulty lifting the front part of the foot, which can cause dragging of the foot or toes along the ground while walking. While foot drop can result from various neurological conditions or injuries, it is not typically associated with loss of consciousness following a motor vehicle accident. Loss of consciousness after a motor vehicle accident is more indicative of potential head trauma or concussion, which may present with symptoms such as altered level of consciousness, headache, pupillary changes, or difficulty waking. Foot drop would be more relevant to assess in contexts related to peripheral nerve injury, spinal cord injury, or neurological conditions affecting the lower extremities. Given the scenario provided, foot drop is not a typical manifestation that the nurse would assess for immediately following a motor vehicle accident with loss of consciousness. Therefore, option E is not relevant in this scenario.
A nurse is teaching a client who has a spinal cord injury about prevention of atelectasis. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A Reason:
"Do panting breaths several times a day." This statement is inappropriate. Panting breaths involve rapid, shallow breathing similar to what a dog does when it's hot. This technique may not be as effective in clearing mucus or promoting lung expansion compared to deep coughing. While panting breaths may have some benefits in promoting ventilation and increasing lung volume, they may not be as targeted or efficient in preventing atelectasis as other techniques such as deep coughing
Choice B Reason:
"Perform deep coughing twice a day." This statement is correct. Deep coughing helps clear mucus and secretions from the airways, reducing the risk of blockages that can lead to atelectasis. It promotes airway clearance and lung expansion, maintaining respiratory function. Regular deep coughing is particularly important for individuals with spinal cord injuries, as they may have impaired cough reflexes or weakened respiratory muscles, increasing their vulnerability to atelectasis.
Choice C Reason:
"Strengthen your chest muscles by performing therapy exercises." This statement is incorrect. While strengthening chest muscles through therapy exercises can be beneficial for overall respiratory health, it may not directly target the prevention of atelectasis. Atelectasis is primarily caused by the collapse of lung tissue due to mucus buildup or reduced lung expansion, rather than weakness of chest muscles. While therapy exercises may have other benefits such as improving respiratory function and endurance, they may not be the most effective strategy for preventing atelectasis in individuals with spinal cord injuries.
Choice D Reason:
"Get plenty of rest throughout the day." This statement is incorrect. Rest is important for overall health and well-being, but it may not directly contribute to the prevention of atelectasis. Inactivity and prolonged bed rest can actually increase the risk of atelectasis by reducing lung expansion and promoting mucus accumulation in the airways. While adequate rest is necessary for recovery and energy conservation, it should be balanced with activities that promote lung expansion and airway clearance, such as deep breathing exercises and mobility.
A nurse is teaching a client who has a complete spinal cord injury about bowel and bladder management. Which of the following instructions should the nurse include in the teaching? (Select all that apply.)
(Select All that Apply.)
Explanation
Choice A Reason:
"It will be necessary to take a stool softener to keep you from becoming constipated." This instruction is correct. Individuals with spinal cord injuries often experience bowel dysfunction, including constipation, due to decreased mobility and impaired bowel function. Stool softeners can help soften the stool and facilitate easier bowel movements, reducing the risk of constipation and associated complications such as fecal impaction.
Choice B Reason:
"Suprapubic catheterization might have to be done if you are unable to catheterize yourself." This instruction is correct. Suprapubic catheterization involves the insertion of a catheter through the abdominal wall directly into the bladder to drain urine. It may be necessary if the client is unable to perform intermittent catheterization independently or if other methods of bladder management are ineffective or contraindicated.
Choice C Reason:
"You will need to learn how to do self-intermittent catheterization to drain your bladder." This instruction is correct. Self-intermittent catheterization involves inserting a catheter into the bladder to drain urine at regular intervals. It is a commonly used method of bladder management for individuals with spinal cord injuries to prevent urinary retention and bladder distention.
Choice D Reason:
"Do not drink fluids excessively as this may cause diarrhea," is not typically included in bowel and bladder management instructions for individuals with spinal cord injuries. Hydration is important for overall health and may help prevent complications such as urinary tract infections, kidney stones, and constipation. Therefore, option D is not appropriate for inclusion in the teaching for a client with a complete spinal cord injury.
Choice E Reason:
"To achieve a bowel movement, daily digital stimulation will need to be done." This instruction is incorrect. Digital stimulation involves gently stimulating the rectum with a lubricated gloved finger to initiate a bowel movement. It can help individuals with spinal cord injuries who have neurogenic bowel dysfunction to stimulate bowel motility and facilitate bowel evacuation.
Which of the following could the nurse expect to observe in an older adult client who has a pneumothorax?
Explanation
Choice A Reason:
Higher oxygen saturations of 98% to 99% is inappropriate. A pneumothorax involves the presence of air in the pleural space, which can compromise lung function and gas exchange. This compromised lung function typically leads to decreased oxygenation of the blood, resulting in lower oxygen saturations rather than higher saturations.
Choice B Reason:
Lower oxygen saturations of 93% to 94% is appropriate. A pneumothorax disrupts the normal exchange of oxygen and carbon dioxide in the lungs due to partial or complete lung collapse. As a result, the affected lung is unable to adequately oxygenate the blood, leading to lower oxygen saturations, which are indicative of hypoxemia.
Choice C Reason:
Lower energy expenditure is inappropriate. Energy expenditure is not typically affected by a pneumothorax. While the discomfort and respiratory distress associated with a pneumothorax may cause the individual to limit physical activity, there is no direct impact on overall energy expenditure.
Choice D Reason:
Increased lung capacity is inappropriate. A pneumothorax results in partial or complete collapse of the affected lung, reducing lung capacity rather than increasing it. The presence of air in the pleural space creates positive pressure, which can compress the lung and decrease its ability to expand fully during inhalation.
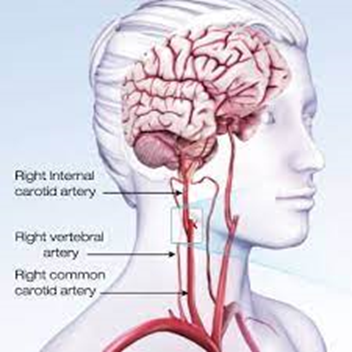
A nurse is caring for a client in the emergency department who has a preliminary diagnosis of a transient ischemic attack (TIA). Which of the following diagnostic testing should the nurse anticipate the provider to prescribe?
Explanation
Choice A Reason:
Prothrombin time (PT) is a laboratory test that measures the time it takes for blood to clot is incorrect. While PT may be part of a comprehensive evaluation in some cases, it is not typically the initial diagnostic test performed for a TIA. A TIA is caused by a temporary disruption of blood flow to the brain, often due to an embolus or transient blockage in a cerebral artery, rather than a primary disorder of blood clotting.
Choice B Reason:
Complete blood count (CBC) is incorrect. A complete blood count (CBC) is a common laboratory test that evaluates the cellular components of the blood, including red blood cells, white blood cells, and platelets. While CBC can provide valuable information about hematological conditions such as anemia or thrombocytosis, it is not specific to diagnosing the cause of a TIA. TIA is primarily a vascular event related to transient ischemia in the brain rather than a disorder of blood cell counts.
Choice C Reason:
Computerized tomography angiography (CTA) is appropriate. CTA is a non-invasive imaging test that combines computed tomography (CT) scanning with contrast dye to visualize blood vessels throughout the body, including those in the brain. CTA can help identify any blockages, narrowing, or abnormalities in the blood vessels supplying the brain, which may be contributing to the TIA. It provides detailed images of the blood vessels' structure and can help guide further management and treatment decisions.
Choice D Reason:
Transesophageal echocardiogram (TEE) is inappropriate. Transesophageal echocardiogram (TEE) is an imaging test that provides detailed images of the heart and major blood vessels using sound waves. While TEE may be indicated in some cases of TIA to evaluate for potential cardiac sources of emboli (blood clots), such as atrial fibrillation or cardiac valve abnormalities, it is not typically the first-line diagnostic test performed in the emergency department setting for evaluating a TIA. Initial imaging studies such as CTA or magnetic resonance imaging (MRI) of the brain are usually prioritized to assess for acute changes in cerebral blood flow and potential causes of the TIA.
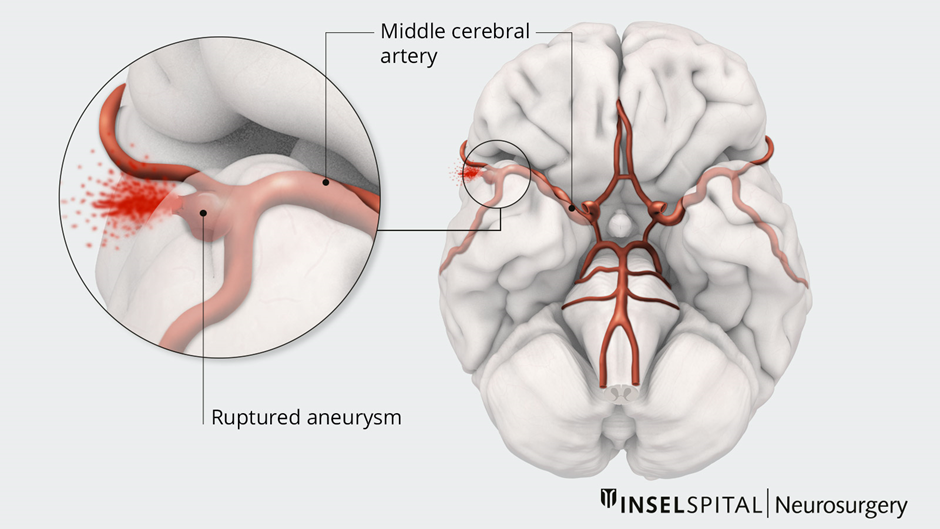
A nurse is providing care for a client who is at risk of cerebral aneurysm rupture. Which of the following interventions should the nurse include in the care plan?
Explanation
Choice A Reason:
Keeping lights turned to medium level in the evening is incorrect. This intervention is aimed at reducing environmental stimuli, which may be appropriate for some patients with neurological conditions to minimize sensory overload and promote rest. However, it is not a specific intervention for preventing cerebral aneurysm rupture.
Choice B Reason:
Maintaining the head of the bed between 30 and 45° is correct. Keeping the head of the bed elevated can help reduce intracranial pressure and decrease the risk of cerebral aneurysm rupture or rebleeding in patients with aneurysmal subarachnoid hemorrhage. This position promotes venous drainage from the brain and helps prevent increases in intracranial pressure.
Choice C Reason:
Administering hypotonic intravenous solutions is incorrect. Hypotonic intravenous solutions have a lower osmolarity than blood plasma and can lead to cerebral edema, which may exacerbate intracranial pressure and increase the risk of cerebral aneurysm rupture. Isotonic solutions, such as normal saline (0.9% NaCl) or lactated Ringer's solution, are typically preferred for fluid resuscitation and maintenance in patients at risk of cerebral aneurysm rupture.
Choice D Reason:
Reposition the client every shift is incorrect. Repositioning the client every shift helps prevent complications associated with immobility, such as pressure ulcers, pneumonia, and venous thromboembolism. While important for overall patient care, repositioning alone does not directly address the risk of cerebral aneurysm rupture.
A nurse is caring for a client who has a transection of the spinal cord at the level of cervical 7. Which of the following assessment findings should the nurse anticipate?
Explanation
Choice A Reason:
The client has no sensation or movement below the level of the injury is correct. This is a characteristic finding of a complete spinal cord injury, where there is total loss of sensory and motor function below the level of the injury. This pattern is often seen in injuries involving the cervical spinal cord, such as at the level of C7.
Choice B Reason:
The client has some movement but no sensation below the level of the injury is incorrect. This finding would be more indicative of an incomplete spinal cord injury, where there is partial preservation of sensory or motor function below the level of the injury. However, with a transection of the spinal cord at C7, it is less likely for the client to have retained movement below the level of injury.
Choice C Reason:
The client has some movement and also some sensation below the level of the injury is incorrect. This finding is not typically associated with a spinal cord injury at the level of C7. With a transection of the spinal cord at this level, there is typically complete loss of sensory and motor function below the level of the injury.
Choice D Reason:
The client has some sensation but no movement below the level of the injury is incorrect. This finding is more consistent with an incomplete spinal cord injury, where there may be partial preservation of sensory function but no motor function below the level of the injury. However, with a transection of the spinal cord at C7, it is less likely for the client to have retained sensation below the level of injury.
You just viewed 10 questions out of the 82 questions on the ATI Medical surgical Exam 1 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



