PEDIATRICS EXAM 4
ATI PEDIATRICS EXAM 4
Total Questions : 35
Showing 10 questions Sign up for moreAn 8-year-old patient presents to his clinic, complaining of dizziness, headaches, and epistaxis. The nurse took the patient's vital signs and noticed that he had high blood pressure in his arms and bounding upper extremity pulses; however, when she proceeded to check his lower extremity pulses, they were weak, and his legs were pale and cool to touch. What does this patient present signs of?
Explanation
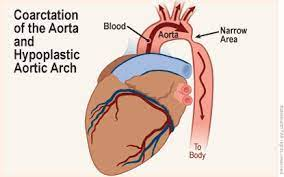
Coarctation of the aorta is a congenital heart defect where the aorta, the major blood vessel that carries oxygenated blood from the heart to the body, is narrowed. As a result, blood pressure tends to be higher in the arms and upper body but lower in the lower body, including the legs. This condition can lead to symptoms such as dizziness, headaches, and even nosebleeds due to high blood pressure. Weak or absent lower extremity pulses, as well as pale and cool legs, are characteristic physical findings in coarctation of the aorta.
A. Tetralogy of Fallot: This is a different congenital heart defect characterized by a combination of four specific heart defects, including ventricular septal defect, right ventricular hypertrophy, pulmonary stenosis, and an overriding aorta. It typically does not cause the symptoms described in the scenario.
C. Pulmonic Stenosis: This condition involves the narrowing of the pulmonary valve or artery, leading to restricted blood flow from the right ventricle to the pulmonary artery. While it can cause various symptoms, it typically doesn't cause the specific blood pressure discrepancies described.
D. Tricuspid Atresia: This is a congenital heart defect where the tricuspid valve is absent or abnormally developed. It leads to the mixing of oxygenated and deoxygenated blood in the heart. While it can cause cyanosis (bluish skin due to low oxygen levels), it doesn't typically cause the specific blood pressure findings mentioned.
An 8-month-old infant has a hypercyanotic spell while blood is being drawn. What is the priority nursing action?
Explanation
Hypercyanotic spells, also known as "Tet spells," can occur in infants with congenital heart defects, particularly tetralogy of Fallot. During these spells, there is a sudden decrease in oxygen saturation, leading to cyanosis (blueness) of the infant's skin and lips, as well as respiratory distress and possible loss of consciousness.
The knee-chest position is a specific technique used to manage hypercyanotic spells. Placing the child in this position helps improve oxygenation by increasing systemic vascular resistance and reducing the degree of right-to-left shunting of blood in the heart. It also increases venous return to the heart, which can help improve cardiac output.
Now, let's discuss why the other options are incorrect:
A. Prepare family for imminent death: This is not the priority action. While hypercyanotic spells can be life-threatening, the immediate focus should be on managing the spell to improve oxygenation and prevent further deterioration. Preparing the family for death should only be considered if resuscitation measures fail, which is not the first-line intervention.
C. Assess for neurologic defects: Assessing for neurologic defects is important but not the immediate priority during a hypercyanotic spell. The primary concern at this moment is addressing cyanosis and respiratory distress to ensure the infant receives adequate oxygen.
D. Begin cardiopulmonary resuscitation: Initiating CPR is not the initial priority during a hypercyanotic spell. CPR would be indicated if the infant's condition deteriorates to the point of cardiac arrest, but it should not be the first step. Placing the child in the knee-chest position is a non-invasive intervention that should be attempted before considering CPR.
Which of the following options gives a nurse the most accurate diagnostic picture of a cardiac issue?
Explanation
B. Cardiac Catheterization.
Cardiac Catheterization (B): Cardiac catheterization is an invasive procedure that involves threading a catheter into the heart's chambers and major blood vessels. It allows direct visualization of the coronary arteries, measurement of blood pressure within the heart, assessment of blood flow, and the ability to perform interventions such as angioplasty or stent placement. Cardiac catheterization is considered the gold standard for diagnosing coronary artery disease, evaluating heart valve function, and detecting congenital heart abnormalities.
Explanation:
A. Echocardiogram (A): An echocardiogram is a non-invasive imaging test that uses sound waves to create images of the heart. It is excellent for assessing the structure and function of the heart, including heart valve function and blood flow patterns. While it is a valuable tool for cardiac assessment, it may not provide the level of detail and direct visualization that cardiac catheterization offers.
C. Chest X-Ray (CXR) (C): A chest X-ray can provide information about the size and shape of the heart and detect certain abnormalities such as an enlarged heart or fluid in the lungs. However, it may not offer the level of detail required to diagnose specific cardiac issues accurately.
D. Electrocardiogram (ECG) (D): An ECG records the electrical activity of the heart and is useful for diagnosing arrhythmias and certain conduction abnormalities. While it provides essential information about cardiac rhythm, it does not directly visualize the structural aspects of the heart or blood flow.
In summary, while each of these diagnostic tools plays a crucial role in assessing cardiac issues, cardiac catheterization is the most accurate and comprehensive option for diagnosing a wide range of cardiac conditions due to its direct visualization and intervention capabilities. However, the choice of diagnostic test should always be made based on the patient's specific clinical presentation and the suspected cardiac problem.
in a non-potty trained child with nephrotic syndrome is the best way to detect fluid retention?
Explanation
A. Weighing the child daily (A) is the most accurate and objective method for monitoring fluid retention in a child with nephrotic syndrome. Nephrotic syndrome can lead to significant fluid retention due to proteinuria and hypoalbuminemia. Daily weight measurements can detect even small changes in body weight, which may be indicative of fluid accumulation. It is a sensitive and specific measure for assessing fluid status.
B. Measuring the abdominal girth weekly (B) can provide some information about abdominal distension, but it is not as precise or sensitive as daily weight measurements. Weight gain or loss can occur without significant changes in abdominal girth, especially in children.
C. Counting the number of wet diapers (C) may provide some information about urinary output, but it does not directly measure overall fluid retention or body weight changes. It is not as reliable as daily weight measurements for assessing fluid status.
D. Testing the urine for hematuria (D) is a valuable diagnostic test to assess kidney function and the presence of blood in the urine, but it does not directly measure fluid retention. Hematuria is not typically the primary indicator of fluid overload in nephrotic syndrome.
In summary, daily weight measurements are the best way to monitor fluid retention in a child with nephrotic syndrome, as they provide a direct and objective assessment of changes in fluid status. This allows healthcare providers to make timely adjustments to the child's treatment plan if necessary.
A 10-year-old has undergone a cardiac catheterization. At the end of the procedure, the nurse should first assess
Explanation
Assessing pulses is a critical step immediately after a cardiac catheterization procedure because it helps determine the adequacy of blood flow to the extremities and any potential vascular complications. Cardiac catheterization involves the insertion of a catheter through blood vessels, which can temporarily affect blood flow. Checking pulses in the affected limb (e.g., the leg or arm where the catheter was inserted) is essential to detect any signs of vascular compromises, such as decreased or absent pulses, which could indicate complications like arterial thrombosis or embolism. Prompt recognition of such issues is crucial for timely intervention to prevent potential complications or limb damage.
The other options are also important but should be addressed after the initial assessment of pulses:
A. Pain: Assessing pain is important, but it should come after checking pulses. If the child reports pain, it could indicate discomfort or complications related to the procedure, which may require further evaluation and intervention.
C. Catheterization report: Reviewing the catheterization report is necessary for a comprehensive understanding of the procedure and its findings, but it is not the immediate priority when assessing the child's post-procedure condition.
D. Hemoglobin and hematocrit levels: Checking hemoglobin and hematocrit levels is important to monitor for potential bleeding complications that may occur during or after the procedure, but it is a secondary assessment compared to evaluating pulses. If there are significant changes in these levels, they may require further investigation and intervention.
In summary, assessing pulses is the initial priority after a cardiac catheterization procedure in order to promptly identify any vascular issues or complications that need immediate attention.
Nick was diagnosed with Hypoplastic Left Heart Syndrome. Which of the following responses should the nurse educate his parents regarding the treatment of this disease?
Explanation
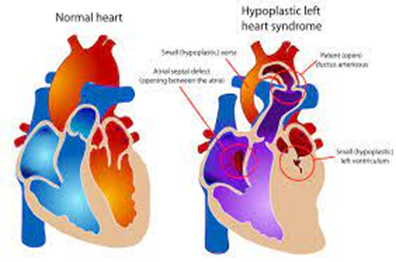
Hypoplastic Left Heart Syndrome is a complex congenital heart defect in which the left side of the heart (left ventricle and aorta) is underdeveloped, making it unable to pump oxygenated blood effectively to the body. The treatment of HLHS typically involves a series of surgical interventions because it cannot be cured with a single surgery. The ultimate goal of treatment is to provide palliative care, which means managing the condition to improve the child's quality of life while waiting for a heart transplant. The surgical procedures are typically performed in stages, with the first surgery usually performed shortly after birth, followed by additional surgeries as the child grows.
Option B is not accurate because HLHS cannot be cured with a single surgery, and creating an opening between the atria and ventricles (e.g., the Norwood procedure) is one step in the staged surgical treatment, but it doesn't completely "cure" the condition.
Option C is not accurate because HLHS is primarily characterized by an underdeveloped left ventricle and aorta, not the displacement of the pulmonary and aortic arteries.
Option D refers to the use of prostaglandin to maintain a patent ductus arteriosus (PDA) and improve blood flow to the lungs, which can be part of the initial management of HLHS but is not a definitive treatment. Prostaglandin is used to stabilize the infant before surgical interventions are performed.
Archie who weighs 44 tb has been given an order for amoxilin 500 mg bid to take before a dentist appointment based on his history of infective endocans. The drug test shows that the daily dose of amoecitin is 50 mg/kg/day in two divided doses. What dose in milligrams is safest for this child?
Explanation
To calculate the safest dose of amoxicillin for Archie based on his weight of 44 pounds (lbs) and the recommended dose of 50 mg/kg/day in two divided doses, you should follow these steps:
Step 1: Convert Archie's weight from pounds (lbs) to kilograms (kg).
1 pound = 0.453592 kilograms
44 lbs * 0.453592 kg/lb = 19.504 kg (rounded to the nearest tenth)
Step 2: Calculate the total daily dose based on his weight.
Total daily dose = Weight (kg) * Dose (mg/kg/day)
Total daily dose = 19.504 kg * 50 mg/kg/day = 975.2 mg/day
Step 3: Divide the total daily dose into two equal doses since it's to be administered in two divided doses.
Each dose = Total daily dose / 2
Each dose = 975.2 mg/day / 2 = 487.6 mg/dose
Since it's not possible to administer a fraction of a milligram accurately, you would round the dose to the nearest available dosage strength.
Therefore, the safest dose for Archie would be:
500 mg
So, Archie should take 500 mg of amoxicillin before his dentist appointment.
Which of the following would Nurse Tony supposed to regard as a cardinal manifestation or symptom of digoxin toxicity to his patient Clay diagnosed with heart failure?
Explanation
Digoxin is a medication commonly used to treat heart failure and certain heart rhythm disorders. However, it has a narrow therapeutic window, and digoxin toxicity can occur if the drug accumulates in the body to excessive levels. One of the hallmark signs of digoxin toxicity is severe bradycardia, which means an abnormally slow heart rate. Bradycardia can result from the effects of digoxin on the electrical conduction system of the heart, leading to an irregular or slowed heartbeat.
While other symptoms can occur in digoxin toxicity, such as gastrointestinal symptoms (like nausea and vomiting), neurological symptoms (like confusion and visual disturbances), and even respiratory distress in severe cases, extreme bradycardia is a key and often life-threatening sign that requires immediate medical attention.
Constipation (A) and headache (C) can also occur as side effects of digoxin but are less specific to digoxin toxicity and may not be considered cardinal manifestations.
Respiratory distress (B) may occur if the bradycardia leads to inadequate cardiac output, causing pulmonary congestion, but it is not a primary or cardinal symptom of digoxin toxicity. Extreme bradycardia is typically the more immediate and prominent concern.
The nurse is evaluating a female child with acute post-streptococcal glomerulonephritis for signs of improvement. Which finding typically is the earliest sign of improvement?
Explanation
APSGN is characterized by inflammation of the glomeruli in the kidneys, which can lead to decreased kidney function and impaired urine output. As the condition begins to improve, one of the first signs is an increase in urine output. This is because the inflammation in the glomeruli starts to resolve, allowing the kidneys to filter blood more effectively and produce a higher volume of urine.
Now, let's discuss why the other options are incorrect:
A. Increased energy levels: While improved energy levels can be a positive sign in a child recovering from an illness, they are not typically the earliest sign of improvement in APSGN. Energy levels may improve as the child's overall condition gets better, but this improvement often follows an increase in urine output.
B. Decreased diarrhea: APSGN primarily affects the kidneys, not the gastrointestinal tract. Therefore, diarrhea is not a direct symptom of this condition. Improving kidney function and urine output would not directly impact diarrhea.
D. Increased appetite: Like increased energy levels, an improved appetite can be a positive sign in recovery, but it is not typically the earliest sign of improvement in APSGN. It is generally more related to overall recovery and feeling better after the acute phase of the illness.
In summary, while all of these signs can be positive indicators of a child's recovery, increased urine output is usually the earliest and most specific sign of improvement in acute post-streptococcal glomerulonephritis, as it directly reflects the resolution of kidney dysfunction.
Surgical repair for patent ductus arteriosus (PDA) is done to prevent the complication of
Explanation
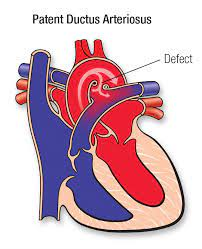
PDA is a congenital heart defect where a blood vessel called the ductus arteriosus, which is supposed to close shortly after birth, remains open. This allows oxygenated blood from the aorta to flow back into the pulmonary artery, leading to increased pulmonary blood flow and congestion. Over time, this can lead to increased pulmonary vascular congestion and potentially cause complications such as pulmonary hypertension and heart failure.
Surgical repair of PDA, often through a procedure known as ligation or closure of the ductus arteriosus, is performed to stop this abnormal blood flow and prevent the associated complications, particularly the increase in pulmonary vascular congestion.
The other options (B, C, and D) are not the primary complications associated with PDA and surgical repair is not performed primarily to address these issues:
B. Decreased workload on the left side of the heart is not a primary reason for surgical repair of PDA, although it can be a potential benefit of closing the ductus arteriosus.
C. Pulmonary infection is not a direct complication of PDA, but the increased pulmonary blood flow associated with a large PDA can make the lungs more susceptible to respiratory infections.
D. Right-to-left shunt of blood is not a typical complication of PDA. PDA typically involves left-to-right shunting of blood, with oxygenated blood flowing back into the pulmonary circulation, leading to complications related to increased pulmonary blood flow.
You just viewed 10 questions out of the 35 questions on the ATI PEDIATRICS EXAM 4 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



