Final Exam OB + Community
Final Exam OB + Community
Total Questions : 60
Showing 10 questions Sign up for moreWhat is the highest priority nursing intervention when admitting a pregnant woman who has experienced a bleeding episode in late pregnancy?
Explanation
Assessing fetal heart rate (FHR) and maternal vital signs would be the highest priority nursing intervention when admitting a pregnant woman who has experienced a bleeding episode in late pregnancy. This is because fetal distress or maternal instability may require immediate medical intervention, such as delivery via emergency cesarean section or blood transfusions, respectively.
Therefore, assessing the FHR and maternal vital signs will help to determine the urgency of the situation and guide the next steps in the management of the patient. Once the patient's condition has stabilized, performing venipuncture for hemoglobin and hematocrit levels, monitoring uterine contractions, and placing clean disposable pads to collect any drainage can be done as appropriate.
A patient arrives at OB triage with a complaint of vaginal bleeding. The nurse would prioritize all of the following questions during the assessment except:
Explanation
The question that the nurse would prioritize the least during the assessment is "Do you plan to have a vaginal or cesarean delivery?" This is because the priority at this point is to determine the urgency of the situation and assess the patient's current condition. The patient's delivery plan can be addressed later after the initial assessment is completed and the patient's stability has been established.
The other questions are all important in determining the cause and severity of the bleeding and the appropriate course of action. The question about the number of weeks is important to determine the gestational age and potential causes of bleeding, as some causes are more common in certain stages of pregnancy. The question about pain can help to determine the possible causes of bleeding and the patient's comfort level. The question about the last ultrasound is important to determine the location of the placenta and whether there are any abnormalities or potential complications.
A woman presents to the emergency department complaining of bleeding and cramping. The initial history is significant for a last menstrual period 6 weeks ago. On sterile speculum examination, the care provider finds that the cervix is closed. The anticipated plan of care for this woman would be based on a probable diagnosis of which type of spontaneous abortion?
Explanation
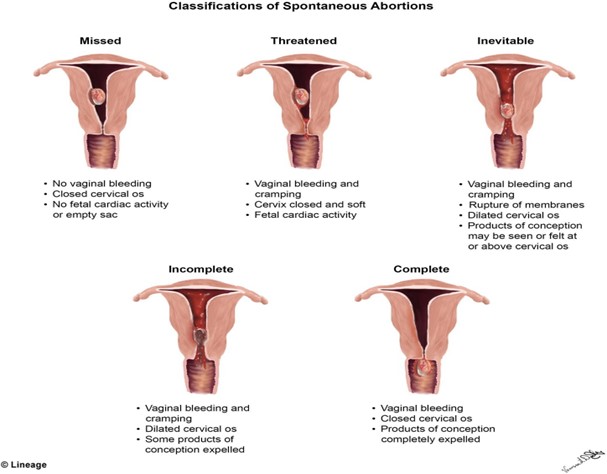
Based on the provided information, the probable diagnosis for the spontaneous abortion in this woman would be a threatened abortion, since the cervix is closed and there is no evidence of expulsion of fetal or placental tissue. A threatened abortion is defined as vaginal bleeding occurring before the 20th week of gestation, with a closed cervical os, and no expulsion of fetal or placental tissue.
The other types of spontaneous abortion are defined as follows:
B. Inevitable abortion: vaginal bleeding and cramping with an open cervical os, with or without expulsion of fetal or placental tissue
C. Missed abortion: fetal demise without expulsion of fetal tissue, and may be associated with a closed cervical os and absence of uterine contractions
D. Incomplete abortion: partial expulsion of fetal or placental tissue, with or without vaginal bleeding, and may be associated with an open cervical os and uterine contractions
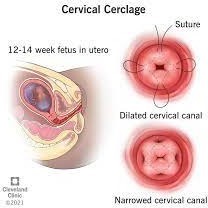
A pregnant woman is being discharged from the hospital after the placement of a cervical cerclage because of a history of recurrent pregnancy loss, secondary to an incompetent cervix. Which information regarding postprocedural care should the nurse emphasize in the discharge teaching?
Explanation
The information that the nurse should emphasize in the discharge teaching for a pregnant woman who has undergone a cervical cerclage due to an incompetent cervix is that the presence of any contractions, rupture of membranes (ROM), or severe perineal pressure should be reported to her healthcare provider immediately. This is because these symptoms could indicate cervical dilation or premature labor, which can lead to pregnancy loss or other complications.
Reporting any vaginal discharge is important, but it is not the most critical symptom to monitor for after cervical cerclage placement. Vaginal discharge is common after cervical cerclage and can occur for several weeks without posing a significant risk to the pregnancy.
A cesarean birth may or may not be necessary depending on the patient's individual circumstances and the course of the pregnancy. It is not a given that all women with cervical cerclage require a cesarean delivery.
While some activity restrictions may be necessary after cervical cerclage placement, it is not necessary for the patient to arrange for care at home. Many women are able to manage their daily activities with appropriate precautions and guidance from their healthcare provider.
Readiness for induction of labor is assessed by determining the:
Explanation
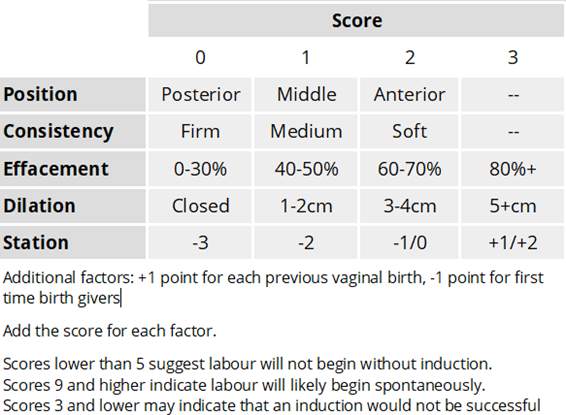
The readiness for induction of labor is assessed by determining the Bishop score. The Bishop score is a system used to evaluate the cervix for induction of labor readiness. It is based on the assessment of five factors: cervical dilation, cervical effacement, cervical consistency, cervical position, and fetal station. Each factor is scored on a scale of 0 to 3, with a maximum possible score of 15.
The higher the Bishop score, the more favorable the cervix is for induction of labor, and the higher the likelihood of a successful vaginal delivery. A Bishop score of 8 or higher is considered favorable for induction of labor. A low Bishop score may indicate that the cervix is not yet ripe and may need further cervical ripening before induction can be attempted.
The Apgar score is a test used to evaluate a newborn's physical condition at birth, based on five factors: appearance, pulse, grimace, activity, and respiration.
The biophysical profile is a prenatal ultrasound evaluation that assesses fetal well-being by evaluating fetal breathing, fetal movement, fetal tone, amniotic fluid volume, and fetal heart rate. Fetal position is an important consideration during labor, as it can impact the progression and outcome of labor, but it is not used to assess readiness for induction of labor.
During labor a fetus with an average heart rate of 135 beats/min over a 10-minute period would be considered to have:
Explanation
The baseline fetal heart rate is the average heart rate over a 10-minute period, excluding accelerations and decelerations, and is an important indicator of fetal well-being during labor.
A baseline fetal heart rate of 110-160 beats/min is considered normal. A baseline heart rate of less than 110 beats/min is considered bradycardia, which can be a sign of fetal distress or hypoxia. A baseline heart rate greater than 160 beats/min is considered tachycardia, which can also be a sign of fetal distress or hypoxia.
Cervidil (dinoprostone) has been ordered for a pregnant woman at 42 weeks of gestation. The nurse recognizes that this medication will be administered to:
Explanation
Cervidil (dinoprostone) is a medication used to ripen the cervix in preparation for labor induction in women who are at or near term.
Cervidil contains a synthetic form of prostaglandin E2, which helps to soften and thin the cervix, making it easier to dilate and efface during labor. The medication is usually administered vaginally, in the form of a small, flat, rectangular-shaped insert that is placed near the cervix.
The medication is released slowly over time, helping to ripen the cervix gradually.
Cervidil is not used to stimulate the amniotic membranes to rupture, enhance uteroplacental perfusion in an aging placenta, or increase amniotic fluid volume.
Fetal well-being during labor is assessed by:
Explanation
Fetal well-being during labor is assessed by the response of the fetal heart rate (FHR) to uterine contractions (UCs). During labor, the fetal heart rate is monitored to assess the well-being of the fetus. The fetal heart rate should increase in response to fetal movement and contractions, which indicates that the fetus is receiving adequate oxygenation and blood flow. This response is called an "acceleration" in the FHR. However, accelerations alone are not enough to assess fetal well-being during labor. It is the combination of the FHR pattern with the uterine contractions pattern that provides the most information.
In addition to the FHR response to UCs, other factors that may be used to assess fetal well-being during labor include fetal scalp blood sampling, fetal pulse oximetry, and fetal ultrasound. Maternal pain control may help to decrease maternal stress and anxiety during labor, but it is not directly related to fetal well-being. An FHR above 110 beats/min is within the normal range for a fetal baseline heart rate, but it is not enough to assess fetal well-being during labor.
A woman in labor has just received an epidural black. The most important nursing intervention is to:
Explanation
Epidural blocks are commonly used during labor to provide pain relief. However, they can also cause a sudden drop in blood pressure, known as epidural-induced hypotension, which can affect fetal oxygenation and fetal heart rate. Therefore, it is important to monitor maternal blood pressure frequently after an epidural block is administered.
While monitoring the maternal pulse is also important, hypotension is the most common complication of epidural anesthesia and can lead to decreased blood flow to the fetus. Therefore, monitoring maternal blood pressure is the priority.
Monitoring the fetus is also important, but it is not the most important intervention after an epidural block. Limiting parenteral fluids may be necessary in some cases to help prevent or treat hypotension, but it is not always necessary and should be done based on the individual situation.
The nurse recognizes that a nonstress test (NST) in which two or more fetal heart rate (FHR) accelerations of 15 beats/min or more occur with fetal movement in a 20-minute period is:
Explanation
The nurse recognizes that a nonstress test (NST) in which two or more fetal heart rate (FHR) accelerations of 15 beats/min or more occur with fetal movement in a 20-minute period is considered reactive. A reactive NST is a reassuring sign of fetal well-being and indicates that the fetal nervous system and cardiovascular system are intact and functioning appropriately. If a reactive NST is not obtained, further testing or evaluation may be necessary to assess fetal well-being.
You just viewed 10 questions out of the 60 questions on the Final Exam OB + Community Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



