HESI PN fundamentals exam
HESI PN fundamentals exam
Total Questions : 60
Showing 10 questions Sign up for moreReview H and P, nurse's notes, laboratory results, and prescriptions.
Complete the diagram by dragging from the choices area to specify which condition the client is most likely experiencing, two actions the practical nurse (PN) should take to address that condition, and two parameters the PN should monitor to assess the client's progress.
Explanation
- Protein deficiency: The client is post-operative (POD 4) and unable to tolerate solid foods, yet she is drinking full liquids without issue. This dietary limitation, especially after surgery, may not be providing sufficient protein, which is essential for wound healing and overall recovery. The client has a slow-healing surgical wound that is red around the edges with serosanguinous drainage. Protein deficiency can impair the body's ability to heal wounds properly and fight infections.
- Include protein supplement shakes in the client's diet: These shakes can provide the necessary protein without requiring the client to eat solid food, ensuring she gets adequate nutrition to support healing and immune function. Protein is critical in recovery, particularly for wound healing and tissue repair, which is why this intervention is essential.
- Advance diet to regular as tolerated: Once the client is able to tolerate liquids without issue, gradually introducing solid foods will ensure she receives a full spectrum of nutrients, including protein, from different food sources. This will support her overall nutritional needs and help improve the rate of wound healing. This should be done gradually, depending on how well the client tolerates solid food.
- Signs of infection: The client has a surgical wound that is red around the edges and has serosanguinous drainage, which could indicate a potential infection. Given the risk of infection, especially in a slow-healing wound, monitoring for other signs such as increased redness, warmth, or purulent drainage is important.
- Wound healing: Wound healing is a critical parameter to monitor in this patient. Given the client's slow-healing surgical wound and potential for protein deficiency, it’s important to track the progress of healing over time. Delayed healing could signal inadequate nutrition (like protein deficiency) or infection, so regular assessment of the wound will help guide further interventions.
- Iodine deficiency: Iodine deficiency typically affects thyroid function and does not directly contribute to the wound healing problems or the inability to tolerate solid foods seen in this client. There are no signs in the patient's data that suggest thyroid dysfunction or iodine deficiency, making this an unlikely condition.
- Glucose deficiency: While glucose is essential for energy, there is no indication from the client’s current condition or lab values that glucose deficiency is a concern. The client is awake and alert, and there are no signs of hypoglycemia or low blood sugar. The primary issue seems to be a lack of protein, not glucose.
- Sodium deficiency: Sodium deficiency is unlikely because there are no signs of hyponatremia (like confusion, dizziness, or muscle cramps) or fluid imbalance, which would be expected in sodium deficiency. The client does not exhibit signs of hypovolemia, and her laboratory results do not suggest significant sodium imbalances.
- Add table salt to any broth that the client takes: Adding salt is not necessary at this time because the client's sodium levels are not critically low. Sodium supplementation is typically used in cases of hyponatremia or fluid imbalances, which do not appear to be a concern here. The primary focus should be on addressing the protein deficiency.
- Place a feeding tube and start enteral feeds: A feeding tube and enteral feeding are typically reserved for clients who are unable to tolerate any oral intake at all. Since the client is drinking full liquids, it is not necessary to place a feeding tube at this stage. If the client continues to struggle with solid food intake over time, then enteral feeding might be considered, but this is not immediately required based on the information provided.
In assisting a dyspneic client with morning care, which action by the practical nurse (PN) is most important?
Explanation
A. Schedule frequent rest periods during care: Allowing frequent rest periods is crucial for a dyspneic client to prevent exhaustion and worsening of respiratory distress. Spacing activities conserves energy, improves oxygenation, and reduces the workload on the heart and lungs during basic care tasks.
B. Assist the client to a chair before making the bed: Moving the client to a chair may help with bed-making logistics but does not directly address the client’s immediate respiratory needs. Prioritizing respiratory support over convenience is more important in dyspneic clients.
C. Ask the client about his usual morning routine: Understanding a client’s routine can help personalize care but is not the most critical action when dyspnea is present. Ensuring that the client can safely tolerate activities without respiratory compromise takes priority.
D. Encourage the client to participate in the care: Encouragement is helpful for promoting independence but must be balanced carefully. Pushing a dyspneic client to participate too much could lead to fatigue and exacerbate respiratory symptoms
The practical nurse (PN) is providing care for a client with a history of a stroke and who has aphasia. The client is exhibiting restlessness, shallow respirations and is clenching teeth. Which problem should the PN assess further?
Explanation
A. Alteration in comfort: Restlessness, shallow breathing, and clenching teeth are strong indicators of discomfort or pain, especially in a client with aphasia who cannot verbalize needs. Assessing for pain or other sources of distress is the priority to address the client’s immediate comfort and prevent further deterioration.
B. Deficit in diversional activity: While limited activity can impact emotional health, signs like restlessness and physical tension suggest an immediate physical problem rather than boredom or inactivity. Comfort issues must be addressed first before considering diversional needs.
C. Elevated blood pressure: Stroke patients are at risk for hypertension, but restlessness and shallow respirations alone do not directly indicate elevated blood pressure. Blood pressure may rise secondary to pain or distress, but comfort assessment is still the initial focus.
D. Change in blood glucose level: Blood glucose fluctuations can cause changes in mental status or energy levels, but the client’s symptoms of clenching teeth and shallow breathing more strongly point toward discomfort or pain rather than hypoglycemia or hyperglycemia.
The practical nurse (PN) turns a client with right sided paralysis from a supine to a left lateral position. Which bony prominence is most likely to manifest signs of erythema when first turned?
Explanation
A. Sacrum: The sacrum is a common site for pressure ulcers in a supine position, but once the client is turned onto the side, pressure shifts away from the sacrum to lateral body surfaces. It is not the most at-risk area in the new position.
B. Ischial tuberosities: The ischial tuberosities bear weight when sitting, not typically when lying in a lateral position. Therefore, they are less likely to be the first site to show erythema when turned onto the side.
C. Lateral malleolus: The lateral malleolus can be at risk when the lower legs rub against the bed, but it is a smaller surface area and would show signs later compared to larger, more pressure-exposed areas like the iliac crest.
D. Iliac crest: The iliac crest on the side the client is turned onto bears significant pressure in the lateral position. It is a major bony prominence directly exposed to force against the mattress, making it the most likely site to show early erythema.
One week after beginning a new prescription for potassium chloride, a client tells the practical nurse (PN) that there is tingling and numbness in the feet and hands. Which action should the PN take?
Explanation
A. Notify the unit charge nurse of the client's reported symptoms immediately: Tingling and numbness can be signs of hyperkalemia, a serious and potentially life-threatening complication from potassium supplementation. Immediate reporting is necessary for prompt evaluation and intervention to prevent cardiac or neuromuscular complications.
B. Reassure the client that the supplement will soon relieve those symptoms: Symptoms like tingling and numbness are not expected side effects of potassium therapy. Reassurance without investigation could delay necessary medical treatment and worsen the client’s condition.
C. Explain that a calcium supplement may be necessary: Calcium supplementation is not the standard response to symptoms of potassium imbalance. Without a clear diagnosis, recommending additional supplements could complicate the clinical situation further.
D. Encourage the client to decrease the intake of dietary sodium: Although reducing sodium is generally beneficial for health, it does not address the acute issue of possible potassium imbalance causing neuromuscular symptoms. Immediate clinical evaluation takes priority.
An older adult client with a stage one sacral pressure wound is discharged with instructions for home care. Which information should the practical nurse reinforce with the client?
Explanation
A. Apply lotion to sacrum: Applying lotion may help with general skin hydration but does not directly address pressure relief, which is the primary intervention needed to prevent worsening of a stage one pressure injury.
B. Use wet-to-dry dressings daily: Wet-to-dry dressings are used for wounds with necrotic tissue that need debridement. A stage one pressure injury involves intact skin without an open wound, so such dressings are not appropriate.
C. Elevate head of bed 30 degrees: Elevating the head of the bed slightly can reduce aspiration risk but also increases pressure on the sacrum if maintained for long periods. Position changes are more critical to relieve sacral pressure.
D. Change positions every 2 hours: Repositioning every two hours is essential to relieve pressure on the sacrum and promote circulation. This practice helps prevent progression of the pressure injury and is a cornerstone of effective pressure ulcer prevention.
A client on a prescribed full liquid diet has a nursing problem of, "Risk for impaired skin integrity related to reduced oral intake." Which snack would be best to provide this client?
Explanation
A. A liquid nutritional supplement that contains protein: A full liquid nutritional supplement with added protein is best because protein is critical for skin integrity and tissue repair. Supplements also provide balanced calories, vitamins, and minerals necessary to support overall skin health and prevent breakdown.
B. Beef broth, or chicken broth: While broth provides fluids and some electrolytes, it is very low in calories and protein, making it insufficient alone for preventing impaired skin integrity in a client with reduced oral intake.
C. Fortified lowfat milk: Milk offers some protein and nutrients, but a specialized nutritional supplement is more calorie-dense and protein-rich, providing a more comprehensive solution for a client at risk for skin breakdown.
D. Apple or grapefruit juice: Fruit juices offer hydration and some vitamins but lack significant protein and calories. They are inadequate for maintaining skin integrity, especially when protein intake is a primary concern.
A client on a prescribed full liquid diet has a nursing problem of, "Risk for impaired skin integrity related to reduced oral intake." Which snack would be best to provide this client?
Explanation
A. A liquid nutritional supplement that contains protein: A full liquid nutritional supplement with added protein is best because protein is critical for skin integrity and tissue repair. Supplements also provide balanced calories, vitamins, and minerals necessary to support overall skin health and prevent breakdown.
B. Beef broth, or chicken broth: While broth provides fluids and some electrolytes, it is very low in calories and protein, making it insufficient alone for preventing impaired skin integrity in a client with reduced oral intake.
C. Fortified lowfat milk: Milk offers some protein and nutrients, but a specialized nutritional supplement is more calorie-dense and protein-rich, providing a more comprehensive solution for a client at risk for skin breakdown.
D. Apple or grapefruit juice: Fruit juices offer hydration and some vitamins but lack significant protein and calories. They are inadequate for maintaining skin integrity, especially when protein intake is a primary concern.
The practical nurse (PN) observes a client's mouth and lips as seen in the picture. Which follow-up action is most important for the PN to take?
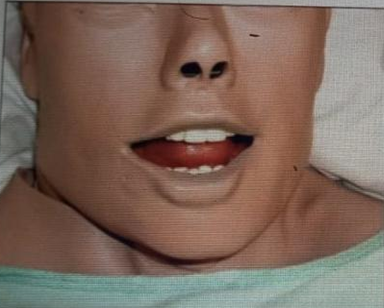
Explanation
A. Offer fluids: Offering fluids is not appropriate when the client shows signs of central cyanosis, as it does not address impaired oxygenation and may pose an aspiration risk if the client is hypoxic or has altered mental status.
B. Administer oxygen: Cyanosis of the lips and tongue indicates poor oxygen saturation and tissue hypoxia. Administering oxygen is the priority action to improve oxygen delivery and prevent respiratory compromise.
C. Ask about pain: While assessing pain is important, it is not the priority in the presence of cyanosis, which reflects a potentially life-threatening oxygenation issue requiring immediate intervention.
D. Provide mouth care: Mouth care is not urgent and does not address the underlying problem of hypoxia. It should be deferred until after the client’s oxygenation status is stabilized.
After accepting employment in a state different from where a practical nurse (PN) is currently employed, it is most important for the PN to review which reference?
Explanation
A. Standards of practice for practical nursing: While important for general nursing care, national or professional standards do not replace the specific legal requirements outlined by the state’s licensing authority, which directly govern what a PN can and cannot do.
B. The licensing state's PN scope of practice: Each state defines the legal scope of practice for practical nurses, including what tasks they are authorized to perform. Reviewing the specific state's scope of practice ensures the PN practices legally and professionally in the new employment setting.
C. Geriatric standards of care guidelines: Geriatric care guidelines help provide quality care for older adults but are not the first priority when ensuring lawful nursing practice across state lines. Legal requirements must be understood first.
D. The employing agency's procedure manuals: While agency policies are important for specific job performance, they must be aligned with the state's legal scope of practice. Knowing the legal boundaries first is crucial before following any workplace procedures.
You just viewed 10 questions out of the 60 questions on the HESI PN fundamentals exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



