Leadership Proctored Exam 2023
ATI Leadership Proctored Exam 2023
Total Questions : 58
Showing 10 questions Sign up for moreA nurse is providing an in-service about client rights for a group of nurses. Which of the following statements should the nurse include in the in-service?
Explanation
a. “A nurse can disclose information to a family member with the client’s permission”
This statement is generally true. In most cases, nurses can disclose information to family members if the client has given consent or if the client lacks decision-making capacity and sharing information with family members is in the client's best interest. However, it's essential to ensure that the client has explicitly granted permission or that sharing information with family members aligns with legal and ethical guidelines, such as those outlined in HIPAA (Health Insurance Portability and Accountability Act).
b. “A nurse is responsible for informing clients about treatment options”
This statement is accurate. Nurses have a responsibility to educate clients about their treatment options, including the benefits, risks, and alternatives, to facilitate informed decision-making. Providing information empowers clients to participate actively in their care and make choices that align with their preferences and values.
c. "A nurse can apply restraints on a PRN basis"
This statement is generally incorrect. The use of restraints on a PRN (as needed) basis should be avoided whenever possible and should only be implemented based on an individualized assessment and with appropriate authorization from a healthcare provider. Restraints should be used as a last resort to ensure the safety of the client or others, and their application must comply with facility policies and regulatory requirements.
d. “A nurse can administer medications without consent to a client as part of a research study”
This statement is incorrect. Administering medications without informed consent violates the principle of autonomy and the rights of the client. In research studies involving human participants, obtaining informed consent is a fundamental ethical requirement. Clients must be fully informed about the nature of the study, potential risks and benefits, and their rights as participants before providing consent. Administering medications without consent would be considered unethical and could lead to serious legal and professional consequences.
A nurse manager observes an assistive personnel incorrectly transferring a client to the bedside commode. Which of the following actions should the nurse take first?
Explanation
a. Help the AP assist the client with the transfer.
While providing immediate assistance to ensure the client's safety is important, it does not address the underlying issue of incorrect technique and may not prevent future occurrences of incorrect transfers.
b. Demonstrate the proper client transfer technique to the AP.
This option addresses the immediate need for correction by providing hands-on guidance to the AP, ensuring that the correct technique is understood and applied in the future.
c. Instruct the AP to request assistance when unsure about a task.
While encouraging the AP to seek assistance when unsure is important, it does not directly address the observed incorrect transfer or provide immediate correction.
d. Refer the AP to the facility procedure manual.
Referring to the procedure manual may provide guidance, but it does not offer immediate correction or ensure that the AP understands and applies the correct technique during client transfers.
A nurse enters a client’s room to witness an informed consent for a gastroscopy. The client states he does not understand the procedure. Which of the following actions should the nurse take?
Explanation
a. Educate the client about the risks of refusing the procedure:
This option suggests providing information about the potential consequences of not undergoing the gastroscopy. While educating the client about risks is essential, the immediate concern is the client's lack of understanding about the procedure itself.
b. Complete the incident report:
Filling out an incident report is typically reserved for situations where there has been an actual incident, such as a medical error or adverse event. In this case, the client's lack of understanding does not constitute an incident but rather a need for clarification.
c. Inform the provider that the client requires clarification about the procedure:
This is the correct action. It involves escalating the issue to the provider responsible for performing the gastroscopy. The provider can then address the client's concerns, answer questions, and provide additional information to ensure informed consent.
d. Answer the client’s questions concerning the procedure:
While answering the client's questions is important, it's not solely the nurse's responsibility to ensure the client understands the procedure. The provider, who will perform the gastroscopy, should be informed of the client's confusion so they can address it effectively.
A nurse is developing a discharge plan for a client who is postoperative and will require a wheelchair in the home. The nurse should place a referral to which of the following resources to assist the client with this need?
Explanation
a. Occupational therapy: Occupational therapists (OTs) specialize in helping people with disabilities or limitations regain independence in performing activities of daily living (ADLs). This includes tasks like bathing, dressing, and mobility. In this case, the OT can assess the client's home environment, recommend wheelchair features or modifications to improve accessibility, and train the client on safe use of the wheelchair in their home setting.
b. Social services: Social services may help with various aspects of the client's discharge plan, such as arranging for home care services, financial assistance, or community resources. While they play a crucial role in addressing broader social determinants of health, such as housing, financial assistance, and community resources, they may not have the expertise or resources to directly address the client's mobility needs related to using a wheelchair.
c. Home health: Home health services typically involve skilled nursing, physical therapy, occupational therapy, and sometimes medical social work delivered in the client's home. While home health services may include physical therapy, the referral specifically for a wheelchair and mobility needs would be more directly addressed by physical therapy.
d. Physical therapy: Physical therapists specialize in movement and mobility and are well-equipped to assess the client's need for a wheelchair, provide training on its safe use, and address any mobility issues that arise. They can also recommend other equipment or exercises to improve the client's mobility and independence. Therefore, a referral to physical therapy is the most appropriate choice in this scenario to assist the client with their mobility needs.While they might be involved in gait training if the client is transitioning from a wheelchair to walking, occupational therapy is more suited for overall functional use of a wheelchair in daily life
A nurse is preparing a teaching session with a client who speaks a different language than the nurse. Which of the following interventions should the nurse plan to include?
Explanation
a. Involve the client’s partner to assist with the teaching session: While involving the client's partner can be helpful, it may not ensure effective communication if the partner also does not speak the same language as the client.
b. Incorporate gestures and hand signals when presenting information: This is an effective strategy to enhance communication with a client who speaks a different language. Non-verbal cues such as gestures and hand signals can help convey meaning and facilitate understanding.
c. Validate understanding by interpreting the client’s body language: Interpreting the client's body language can be helpful in assessing their level of understanding and engagement. However, it may not be sufficient for effective communication, especially if the client has questions or needs clarification.
d. Provide an interpreter when obtaining consent from the client: This is the most appropriate intervention. Using a professional interpreter ensures accurate communication between the nurse and the client, facilitating understanding and ensuring that the client's rights are upheld during the consent process.
A charge nurse is observing a newly licensed nurse use aseptic technique when irrigating a client’s open abdominal wound. The charge nurse should intervene for which of the following actions by the newly license nurse?
Explanation
a. Wears clean gloves to remove the soiled dressing: This action is appropriate. Wearing clean gloves helps maintain aseptic technique and prevents contamination of the wound during dressing removal.
b. Uses slow, continuous pressure to flush the wound: This action is appropriate. Using slow, continuous pressure helps ensure effective irrigation of the wound without causing trauma to the tissue.
c. Places the syringe tip with angiocatheter 2.5 cm (1 in) above the open wound bed: This action is appropriate. Maintaining the appropriate distance ensures that the irrigation solution reaches the wound bed effectively without causing unnecessary trauma.
d. Opens irrigation supplies before removing the soiled dressing: This action is not appropriate. Opening irrigation supplies before removing the soiled dressing increases the risk of contamination. The nurse should first remove the soiled dressing using aseptic technique and then prepare the irrigation supplies.
A nurse is preparing to discharge a client who has end-stage heart failure. The client’s partner tells the nurse she can no longer handle the client. Which of the following actions should the nurse take?
Explanation
a. Contact the case manager to discuss discharge options: This is an appropriate action. The case manager can assist in assessing the client's needs and coordinating appropriate discharge arrangements, such as arranging for home health services or exploring alternative care options.
b. Request another family member assist the client’s partner with care: This may be a helpful action if there is another family member who can provide support. However, it's important to consider the availability and willingness of other family members to take on caregiving responsibilities.
c. Recommend the partner place the client in a long-term care facility: This option may be considered if the partner is unable to continue providing care and there are no other feasible options available. However, it should be discussed with the client and their partner and explored as one of several potential solutions.
d. Ask the provider to delay the client’s discharge home for a few more days: This may be appropriate if there are concerns about the client's safety or if additional time is needed to arrange for alternative care options. However, it's important to address the underlying issues contributing to the partner's inability to provide care and to explore long-term solutions.
A nurse working in an emergency department is performing triage. To which of the following clients should the nurse assign priority?
Explanation
a. A client who reports night sweats and fever for the last week:
Night sweats and fever can be indicative of various underlying conditions, including infections. While these symptoms may require medical attention, they do not necessarily indicate an immediately life-threatening condition compared to other options.
b. A client who has compound fractures of the tibia and humerus:
Compound fractures involve broken bones that penetrate through the skin, leading to a risk of severe bleeding, infection, and other complications. This client's injuries are significant and require immediate attention to prevent further complications and provide pain management and stabilization.
c. A client who reports severe vomiting and diarrhea:
Severe vomiting and diarrhea can lead to dehydration, electrolyte imbalances, and other complications, especially if prolonged or accompanied by other symptoms such as fever. While this client requires prompt assessment and treatment, the urgency may not be as high as for other conditions.
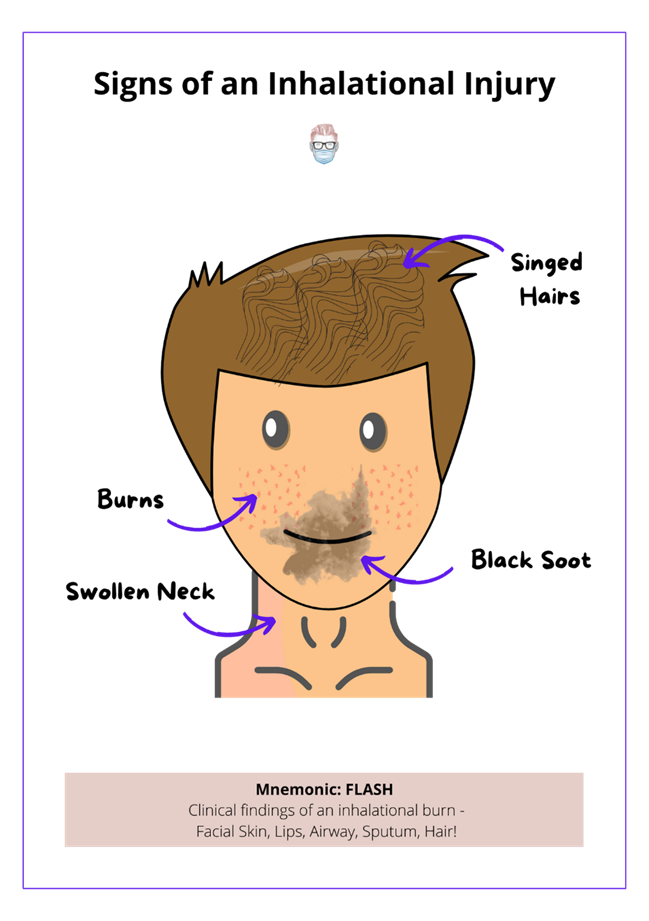
d. A client who has soot markings around each naris following a house fire:
Soot markings around the nares (nostrils) suggest inhalation injury, which can lead to airway compromise, respiratory distress, and other serious complications. This client requires immediate assessment and intervention to ensure airway patency, oxygenation, and respiratory support.
To resolve a conflict between staff members regarding potential changes in policy, a nurse manager decides to implement the changes she prefers regardless of the feelings of those who oppose those changes. Which of the following conflict resolution strategies is the nurse manager using?
Explanation
a. Compromising:
Compromising involves finding a middle ground or mutually acceptable solution where both parties give up something to reach an agreement. It requires each party to make concessions to meet halfway and resolve the conflict. This approach aims to achieve a quick resolution by accommodating the needs and concerns of both sides to some extent.
b. Collaborating:
Collaborating involves working together cooperatively to find a solution that satisfies the interests and concerns of all parties involved. It requires open communication, active listening, and joint problem-solving to achieve a consensus and reach a win-win outcome. This approach values mutual respect, trust, and cooperation among team members, emphasizing shared decision-making and collective ownership of the resolution.
c. Cooperating:
Cooperating involves willingly assisting or supporting others to achieve a common goal or resolve a conflict. It emphasizes teamwork, mutual support, and shared efforts to address challenges or differences constructively. This approach promotes harmony, unity, and a supportive environment where individuals work together toward shared objectives.
d. Competing:
Competing, also known as forcing or dominating, involves pursuing one's own interests or preferences at the expense of others' concerns or viewpoints. It prioritizes assertiveness and control, with the goal of achieving one's desired outcome without considering the needs or perspectives of others. This approach can lead to conflict escalation, resentment, and strained relationships, as it disregards collaboration and mutual understanding in favor of imposing one's will.
A nurse in the emergency department is assessing a client who is unconscious following a motor- vehicle crash. The client requires immediate surgery. Which of the following actions should the nurse take?
Explanation
a. Transport the client to the operating room without verifying informed consent:
This option suggests an urgent response, prioritizing the immediate need for surgery over the formal process of obtaining informed consent. In certain emergency situations, such as when a patient's life or health is in imminent danger and obtaining consent is not feasible, healthcare providers may proceed with treatment or surgery to prevent further harm or loss of life. However, this approach should be guided by established protocols, legal considerations, and the principle of providing the best possible care for the patient.
b. Delay the surgery until the nurse can obtain informed consent:
This option advocates for ensuring that the patient's autonomy and rights are respected by obtaining informed consent before proceeding with surgery. While obtaining consent is essential, delaying surgery may not always be feasible or advisable in emergency situations where prompt intervention is necessary to prevent deterioration of the patient's condition. However, if circumstances allow, making efforts to obtain informed consent is ethically and legally preferable.
c. Obtain telephone consent from the facility administrator before the surgery:
This option proposes seeking consent from a designated authority within the healthcare facility, such as a facility administrator, via telephone. While this approach may be practical in some cases, it may not always be sufficient to ensure that the patient's rights are fully respected, particularly if the administrator does not have the legal authority to provide consent on behalf of the patient. In emergency situations, obtaining consent from a legally authorized representative of the patient, if available, is generally preferred.
d. Ask the anesthesiologist to sign the consent:
This option involves delegating the responsibility of signing the consent form to another member of the healthcare team, in this case, the anesthesiologist. However, consent for surgery should ideally be obtained directly from the patient or their legally authorized representative, as they are the ones who have the right to make decisions about their medical care. Relying on another healthcare provider to sign the consent form may not adequately protect the patient's autonomy and legal rights.
You just viewed 10 questions out of the 58 questions on the ATI Leadership Proctored Exam 2023 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



