Medical Surgery Exam 2
Medical Surgery Exam 2
Total Questions : 43
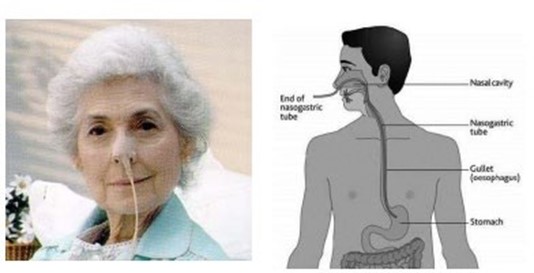
Showing 10 questions Sign up for moreA patient admitted with a peptic ulcer has a nasogastric (NG) tube in place. When the patient develops sudden, severe upper abdominal pain, diaphoresis, and a firm abdomen, which action should the nurse take?
Explanation
The nurse should quickly assess the patient's vital signs to check for signs of shock and instability. If the vital signs are unstable, the nurse should initiate appropriate interventions to stabilize the patient, such as administering oxygen, starting IV fluids, and providing continuous cardiac monitoring. Based on the sudden onset of severe upper abdominal pain, diaphoresis, and a firm abdomen, the nurse should suspect a possible perforation or bleeding related to the peptic ulcer. This is a medical emergency that requires immediate intervention. Therefore, the nurse should prioritize notifying the healthcare provider and preparing the patient for urgent medical evaluation.
Option A, irrigating the NG tube, is not appropriate in this situation and may further exacerbate the patient's condition if the ulcer has perforated.
Option B, elevating the foot of the bed, is also not appropriate as it does not address the patient's current symptoms.
Option C, giving the ordered antacid, may not be effective in addressing the severity of the patient's symptoms and should be postponed until the healthcare provider has evaluated the patient.
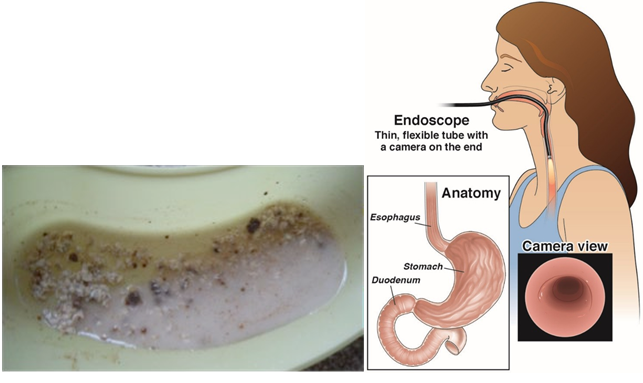
What diagnostic test should the nurse anticipate for an older patient who is vomiting "coffee-ground" emesis?
Explanation
"Coffee-ground" emesis is a term used to describe vomit that has the appearance of coffee grounds, which indicates that the vomit contains partially digested blood. This is a serious symptom that could be indicative of an upper gastrointestinal bleed. An endoscopy is a diagnostic test that allows healthcare providers to visually examine the upper gastrointestinal tract and identify the source of bleeding.
Barium studies and angiography are not typically used to diagnose upper gastrointestinal bleeds. Gastric analysis may be useful in other diagnostic situations, but it is not the most appropriate test for a patient with "coffee-ground" emesis.
A 53-year-old male patient with deep partial-thickness burns from a chemical spill in the workplace has severe pain followed by nausea during dressing changes.
Which action will be most useful in decreasing the patient's nausea?
Explanation
Prochlorperazine is an antiemetic medication that is commonly used to treat nausea and vomiting caused by various conditions, including chemotherapy, radiation therapy, and surgery. Giving the medication before the dressing changes, can prevent or minimize the onset of nausea and vomiting, which can be triggered by the pain and anxiety associated with the procedure.
Option B, keeping the patient NPO (nothing by mouth) for 2 hours before dressing changes, may be helpful in reducing the risk of aspiration if the patient needs sedation or general anesthesia for the procedure. However, it is not directly related to reducing the patient's nausea.
Option C, avoiding performing dressing changes close to the patient's mealtimes, may help reduce the risk of nausea caused by an overly full stomach, but it is not directly related to reducing the patient's nausea during the procedure.
Option D, administering prescribed morphine sulfate before dressing changes, may help reduce the patient's pain during the procedure, but it may also increase the risk of nausea and vomiting as a side effect. Therefore, this option may not be the most useful in decreasing the patient's nausea.
A 26-year-old woman is being evaluated for vomiting and abdominal pain. Which question from the nurse will be most useful in determining the cause of the patient's symptoms?
Explanation
Nausea and vomiting are common symptoms of early pregnancy, and abdominal pain can also occur due to various pregnancy-related conditions. Therefore, it is essential to rule out pregnancy as a potential cause of the patient's symptoms before pursuing other diagnostic options.
Once pregnancy has been ruled out, the nurse can ask additional questions such as those listed in options a, b, and d to further narrow down the potential causes of the patient's symptoms.

Which information will the nurse include when teaching a patient how to avoid chronic constipation? (Select all that apply.)
Explanation
Option b is not entirely correct because while bulk-forming laxatives contain fiber, they may not always be the best source of fiber, and their use should be individualized according to the patient's needs.
Option e is incorrect because while stimulants and saline laxatives can be effective for occasional constipation, they should not be used regularly or for an extended period without medical supervision as they can lead to dependence and other complications.

A patient calls the clinic to report a new onset of severe diarrhea. What should the nurse anticipate that the patient will need to do?
Explanation
The nurse should anticipate that the patient will need to collect a stool specimen. Diarrhea can be caused by various factors such as infections, inflammatory bowel disease, food intolerance, and medication side effects. Collecting a stool specimen can help identify the underlying cause of the diarrhea and guide appropriate treatment. Blood cultures, colonoscopy but barium enema may be necessary in certain cases but are not typically the first step in the diagnostic process for diarrhea.
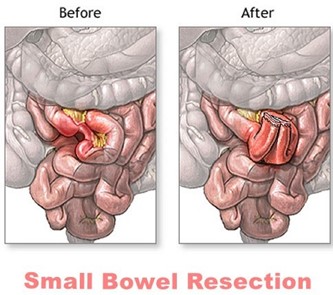
A patient reports gas pains and abdominal distention 2 days after a small bowel resection. Which nursing action should the nurse take?
Explanation
Gas pains and abdominal distention are common postoperative complications following small bowel resection. Ambulation is a simple and effective nursing intervention that can help alleviate these symptoms. Walking helps stimulate peristalsis, which can help move gas and stool through the gastrointestinal tract. It can also help prevent postoperative complications such as pneumonia and deep vein thrombosis.
Administering morphine sulfate (option A) may relieve pain, but it can also worsen constipation and abdominal distention. Promethazine (option C) is an antiemetic medication and may be helpful if the patient is experiencing nausea, but it is not the best intervention for gas pain and abdominal distention. Instilling a mineral oil retention enema (option D) may also be helpful in some cases, but it is not typically the first intervention for these symptoms and should be ordered by a healthcare provider.
A 68-year-old female client is being seen for follow-up wound care on her right lower leg. During her visit, the client states she hasn't had a bowel movement since her last visit a week ago. The client states she hasn't had much of an appetite in the past few days and says, "l figure I don't have anything in there to come out." The nurse auscultates the client's abdomen and hears hyperactive high-pitched bowel sounds in the upper left quadrant and hypoactive bowel sounds in the lower left quadrant. The nurse collaborates with the primary health care provider and the client is directly admitted to the hospital for possible intestinal obstruction. Before going to the hospital, the client asks the nurse what to expect. Which of these statements by the nurse (is) most likely accurate?
Select all that apply.
Explanation
Option A is not the best advice because drinking lots of water alone may not be enough to relieve constipation, especially if there is an obstruction.
Option B is also not accurate because not all intestinal obstructions require surgery, and the treatment approach will depend on the cause and severity of the obstruction.
Option C is accurate because a nasogastric tube can help relieve any distention caused by the obstruction by removing any gas or fluids that may have accumulated in the stomach and small intestine.
Option D is also accurate because an abdominal CT is one of the diagnostic tests that can help confirm the presence of intestinal obstruction and provide information about the location and cause of the obstruction.

A young adult patient is admitted to the hospital for evaluation of right lower quadrant abdominal pain with nausea and vomiting. Which action should the nurse take?
Explanation
The nurse should suggest the patient lie on the side, flexing the right leg². This position may help relieve pain and reduce tension in the abdominal muscles¹. Palpating the abdomen for rebound tenderness (a) may cause pain and should be avoided¹. Assisting the patient to cough and deep breathe (c) may be helpful for respiratory issues but not for abdominal pain¹. Encouraging the patient to sip clear, non-carbonated liquids (d) may be helpful for hydration but does not address the abdominal pain¹.

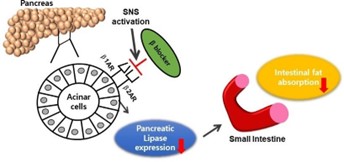
Which laboratory test result will the nurse monitor to evaluate the effects of therapy for a patient who has acute pancreatitis?
Explanation
Lipase is an enzyme that is produced by the pancreas and is involved in the digestion of fats. In acute pancreatitis, the pancreas becomes inflamed, and lipase levels in the blood can become significantly elevated. Monitoring lipase levels can help healthcare providers to assess the severity of pancreatitis, track the effectiveness of treatment, and determine when it is safe to start a patient on a normal diet.
You just viewed 10 questions out of the 43 questions on the Medical Surgery Exam 2 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now